Category: Healthcare Insights
Telepractice Resources
Published by Feeding Matters on Apr 10, 2020
Feeding Matters is committed to providing up-to-date telepractice logistics, technology, delivery, and overall experience resources. The links below will provide you with more information about organizations supporting the move to increased telepractice. You can also visit the Feeding Matters Resource Library to find handout and templates related to telepractice. There is also the opportunity for you to submit any resources that may be helpful to those accessing our website.
Organizations Supporting Telepractice
- Family and Community Resources
- Laws & Regulation Resources
- National Organization Links for Telepractice
- Practice Management
- Telepractice in Assessment & Management
Handouts and Templates
Please visit the Resource Directory for the following resources:
- Billing Guide for Telehealth Encounters
- Email template for First Telehealth Session
- Home Feeding Therapy Kit
- Home OT Kit
- Platform Options
- Preparing for Successful Teletherapy
- Use of Video Conference for Telepractice – A Resource Summary
PFD Alliance Information
Published by Cuyler Romeo on Feb 27, 2020
The PFD Alliance is an open access community of professionals, families and community partners driven to further advances in PFD by accelerating identification, igniting research, and promoting collaborative care.
PFD Alliance at-large members receive PFD Alliance quarterly updates and are invited to participate in Digital Ideations, Symposiums and Town Halls to contribute input for future Alliance actions. Members also may join committees, serve as leadership, complete volunteer projects or give time as they are able through several levels of participation.
Alliance participation levels include:
- The Executive Council: Members who serve in positions of leadership which include: Family Advisory Chair, Medical Director, Pillar Chairs, and Committee Leads
- Pillar Committee Members: Members who serve on the active committees of the Alliance
- Volunteers: Alliance members who engage in specific volunteer actions such as completing special projects or executing events.
- At-Large Members: These members are engaged in the Alliance through communication, surveys, and invitations to our twice-yearly virtual meetings.
To ensure all aspects of care are addressed, we have organized efforts to fall under one of the four pillars within the PFD Alliance: Education, Research, Advocacy, and Support. Although each pillar focuses on a specific area, the goals of each are aligned.
EDUCATION PILLAR
Build a workforce of qualified professionals to evaluate and treat pediatric feeding disorder. We will do this by impacting education that will result in better care, improved health outcomes and enhanced early intervention.
- Conference Committee
- The conference committee works to determine an evidence-based conference agenda along with a featured lightning talk. During the year, the committee works to ensure that the planning of the conference goes well and educational opportunities are of the highest caliber for attendees
- PFD Educational Initiatives Committee
- The PFD Educational Initiatives committee works to understand the educational needs of our feeding community while considering provider and client needs. The Educational Initiative committee strives to develop a professional network for information dissemination while advancing the community’s understanding of PFD across the four domains.
- Resources Committee
- The resources committee works to determine what partnerships need to be built with existing groups to provide more information around pediatric feeding disorder and how Feeding Matters can be the conduit of information. The committee also works to maintain the usability of our website as we investigate areas of improvement.
Grow a network of advocates, including respected clinicians, researchers, caregivers, educators, healthcare professionals, insurance providers and more to influence public policy and facilitate change to improve the lives of children with pediatric feeding disorder.
- PFD Identity:
- Partner with associations and other organizations to support the approval of the ICD
Ignite research to define evidence-based best practices that will lead to better care for infants and children with pediatric feeding disorder.
- Small Grants Committee
- The small grants committee assesses research needs, reviews applications, and grants dollars to researchers interested in moving the field of pediatric feeding disorder forward.
- ICFQ Research Project
- Research the ICFQ to determine if it can be a psychometrically sound screening tool for early identification
Empower families so that they are educated on PFD, equipped with resources, supported to advocate for their child, and to ensure their family receives the best care possible.
- Family Advisory Council
- The Family Advisory Council (FAC) advises Feeding Matters and the PFD Alliance on how to more effectively meet the needs of families navigating pediatric feeding disorder (PFD) – providing feedback on proposed policy, programs, initiatives, and strategic planning. FAC members have a wide variety of experiences with pediatric feeding disorder and represent the diversity of families impacted by PFD.
- Power of Two parent coaching
- Qualified family coaches who have first-hand experience with PFD are matched with families struggling to overcome the medical, emotional, financial, educational, and social issues often faced with PFD. Through shared experiences, Power of Two family coaches offer emotional support, compassion, resources, and guidance – reminding caregivers that they are not alone.
Feeding Matters funds clinical tool research project
Published by Feeding Matters on Feb 14, 2020
Feeding Matters launched its small grants program in 2019 to support the growing need for research on Pediatric Feeding Disorder (PFD). The initiative was led by the Granting Research Committee as a part of Feeding Matters’ Pediatric Feeding Disorder Alliance. The committee’s goal was to advance the PFD field by granting funds to researchers who proposed studies that fill the gaps in PFD research. The committee is delighted to support researchers Paula Rabaey, Ph.D., OTR/L and Kate Barlow, OTD, OTR/L on their project. Their study seeks to address two specific research questions: (1) To what extent do current assessments by feeding clinicians address the four domains of PFD? (Medical, Nutritional, Feeding Skills, and Psychosocial Factors). (2) What are feeding clinicians’ perceptions of current assessment tools used in evaluation and treatment of PFD?
Researcher Bios
 Paula Rabaey, Ph.D., is an Assistant Professor at St. Catherine University in St. Paul, MN. She has 25+ years clinical experience in pediatric occupational therapy including early intervention and feeding, eating, and swallowing. She is a feeding technical expert for SPOON Foundation (http://www.spoonfoundation.org/) and has developed curriculum to train caregivers in orphanages around the world in safely feeding children with disabilities. She recently presented in Tula, Russia on feeding strategies and at the 2nd Annual OT conference in Morocco on pediatric feeding in January 2020.
Paula Rabaey, Ph.D., is an Assistant Professor at St. Catherine University in St. Paul, MN. She has 25+ years clinical experience in pediatric occupational therapy including early intervention and feeding, eating, and swallowing. She is a feeding technical expert for SPOON Foundation (http://www.spoonfoundation.org/) and has developed curriculum to train caregivers in orphanages around the world in safely feeding children with disabilities. She recently presented in Tula, Russia on feeding strategies and at the 2nd Annual OT conference in Morocco on pediatric feeding in January 2020.
Background
The high incidence of pediatric feeding problems is well documented, with a prevalence as high as 25% in typically developing children, 70% in pre-mature children, 80% in children with developmental disabilities (Korth & Rendell, 2015), and over 90% in children with cerebral palsy (Ju Ko, et al., 2011). With the movement to classify the range of feeding problems in the pediatric population into a unifying term “Pediatric Feeding Disorder” (PFD), there is a need for standard guidelines to choose the most appropriate assessment tool(s) that aligns with the four domains of PFD including: medical, nutritional, feeding skills, and psychosocial factors (Goday, 2019). There are many available non-instrumental assessment tools for clinicians to use; however many of the commonly used assessments are site-specific evaluations and parent questionnaires, such as the Sensory Profile and the PediEat. An issue faced by clinicians, is that the objective standardized assessments that are valid and reliable are lacking in the area of pediatric feeding and swallowing (Barton, Bickell & Fucile, 2018; Heckathorn, Speyer, Taylor & Cordier, 2016; Speyer, Cordier, Parsons, Denman & Kim, 2018). A recent systematic review on the psychometric characteristics of 10 non-instrumental pediatric feeding and swallowing assessments found missing, incomplete or conflicting psychometric data for all reviewed (Speyer, Cordier, Parsons, Denman & Kim, 2018). These assessments also were very specific to only one aspect of feeding. Assessment and treatment of PFD is critical in all domains to ensure inter-disciplinary collaboration and positive outcomes for both child and family. The purpose of this study is to investigate assessments currently used by feeding clinicians out in the field, and categorize them by the four domains of PFD in order to better understand current assessment practices and to inform future evidence-based assessment and treatment of PFD.
Methodology
This study will use a mixed methods research design in which both quantitative and qualitative data will be collected via survey research and focus groups in two areas of the United States (Midwest and East coast). The quantitative survey will examine the extent that current feeding assessments fit within the four domains of PFD and the qualitative focus groups will examine clinicians’ perspectives of current assessment tools being used for pediatric feeding problems. Mixed methods research provides a way to approach knowledge from multiple viewpoints, perspectives, and research approaches that allow for greater depth and breadth of understanding the problem (Johnson, Onwuegbuzie, & Turner, 2007). Appropriate sample size will be calculated for the survey research portion, and a smaller sample size of clinicians will be used in the qualitative portion using focus groups. Data will be analyzed by the Co-PI’s using NVivo software, which allows for greater validity of the results. Focus groups will be recorded, transcribed, and analyzed according to grounded theory methodology. Final data analysis includes comparing and contrasting the two data sets in order answer the research questions.
References
Barton, C. Bickell, M., & Fucile, S. (2018). Pediatric oral motor feeding assessments: A systematic review. Physical & Occupational Therapy in Pediatrics, 38(2), 190-209. DOI: 10.1080/01942638.2017.1290734
Goday, P.S., Huh, S.Y., Silverman, A. Lukens, C.T., Dodrill, P., Cohen, S.S…..Phalen, J.A. (2019). Pediatric feeding disorder-consensus definition and conceptual framework. Journal of Pediatric Gastroenterology and Nutrition, 68(1), 124-129.
Heckathorn, D., Speyer, R., Taylor, J., & Cordier, R. (2016). Systematic review: Non-instrumental swallowing and feeding assessments in pediatrics. Dysphagia, 31, 1-23.
Johnson, R.B., Onwuegbuzie, A.J., & Turner, L.A. (2007). Toward a definition of mixed methods research. Journal of Mixed Methods Research, 1(2), 112-133.
Ju Ko, M., Kang, M., Ko, K., Ki, Chang, H., Kwon, J. (2011). Clinical usefulness of Schedule for Oral-Motor Assessment (SOMA) in children with dysphagia. Annals of Rehabilitation Medicine, 35, 477-484.
Korth, K. & Rendell, L. (2015). Feeding Intervention. In J. Case-Smith & J. Clifford O’Brien (Eds.). Occupational therapy for children and adolescents, (7th ed., 389-414). St. Louis, MI: Elseview Mosby.
Speyer, R., Cordier, R., Parsons, L., Denman, D., & Kim, J. (2018). Psychometric characteristics of non-instrumental swallowing and feeding assessments in pediatrics: A systematic review. Dysphagia, 33, 1-14. https://doi.org/10.1007/s/00455-017-9835-x
Holidays reminds me of fun at Grandma’s
Published by Epic Medical Solutions an Aveanna Company on Dec 02, 2019
The holidays reminds me of fun at Grandma’s house: playing with cousins, building with Tinker Toys, sledding so long that our mittens (and fingers!) were frozen solid, and decorating cookies. These sweet memories have a special place in my heart.
The holidays with tube fed children should be equally memorable. In a time of year that seems to be focused on food (chocolate in stocking, decorating cookies, and of course the big family dinner) it may feel like it is impossible to have a “normal” holiday. However, simple modifications can make all the difference for your little one. Here are a few ideas to consider:
- Take the focus off of food. Traditionally, we pack the holiday season with tasty treats. Instead of focusing on edible gifts, try other small toys and unique gifts. Stuff your stockings with hair ties, coupons for a special date with mommy/daddy, craft projects, and toy cars. These small trinkets allow the fun to continue long past when the snacks are devoured.
- It helps to notify the family members who may not know all the details of the health situation, this way there are no awkward questions or pressure about “just try to eat a little mashed potato”. Understanding and compassionate family and friends can really help support caregivers during holiday dinners when they do have more insight on the situation.
- Enjoy nature. Bundle up in warm clothes and head out with friends and family. Sledding, hiking, building snowmen and having snowball fights are all a blast, especially with friends! Just remember to secure the feeding tube so that your child can enjoy the fun without harm to the tube; an emergency run to the hospital puts a damper on snow fun.
- Pack an emergency kit. Don’t forget that winter weather may trap you in at Grandma’s house. Pack plenty of formula and supplies: syringes, gauze, tape, extensions, etc. Don’t forget your pump and charger (and a backup, if you have it!), a backup feeding tube, feeding bags and a gravity bag (in case heavy snow comes and the power fails).
- Have fun! It’s okay to create new family traditions and memories without feeling like you are abandoning tradition. Incorporating more going and doing instead of giving and receiving is great! The holidays is not about the gifts or food, it’s about bringing family close, loving others and celebrating the season
Food Is Sensory: Post-Event Blog
Published by Marsha Dunn Klein on Oct 23, 2019

Post-Event Blog
- Is there a formal assessment that parents and healthcare professionals can use to help “grade the ask” for children who refuse to eat? Do you have any strategies you recommend?
First of all, I believe we need to be careful about the words we use. I, personally, do not usually talk about children “refusing to eat”, and do not chart “refusal behaviors”, as such. I chart other things. I see the adult role as “offering” appropriate foods and children can eat them or not. I do not describe children as “refusing”. I describe them as communicating something to us and we, as their caring grownups, need to play detective and try hard to understand why they are not YET able to eat that food. I think when a child is not taking the food we offer, there is a reason. But, might we be asking too much?
In my new book, I talk about grading our ask. There is not a formal grading the ask assessment, just guidelines. Is the food or liquid safe (and does the child BELIEVE that?) Is the food the right developmental ask? (Is the child developmentally ready for that food, utensil, or eating skill?) Is the food the right sensory ask? (Is the child YET comfortable with the look, smell, sound, texture or taste of that food? Can we modify it so the sensory ask is smaller, more graded, and the child is more motivated to try it?) Is the food the right motor ask? (Does the child have the safe and confident eating skills needed for the food offered?) Is the food the right emotional ask? Can we start where the child feels comfortable and successful and tiptoe from there? If the child has had scary or worrisome experiences with that or similar food or mealtimes in the past, are we pushing him right into LOTS OF WORRY with our ask? Can we scale that back? Are we expecting the right independence ask? Are we requiring the child to eat when WE feed him, when he is perfectly capable of feeding himself?
We could chart refusal behaviors, but maybe “refusal” in that situation is the right response for that child from his perspective. I actually believe I could get ANY child to “refuse” just by the way I presented a food. I look at refusal as MY NEED TO ADAPT, (grade the ask) NOT the child’s need to comply with my demand.
- How do you define a “successful” treatment for a child with a pediatric feeding disorder? Is there criteria you recommend?
Successful treatment for a child, in my opinion, requires the parent to be included as an active participant in the WHOLE process. We need to support families at the pace the child AND PARENT are comfortable. Just like I believe that if the child is “refusing” they are communicating some type of struggle to us, and WE MUST adapt, I also believe if a parent is not successful, then we, as supportive team members must try to understand why, meet the parent where they are at, where they are ready, and re-think how we are offer support. Just like not all treatment strategies work for all children, not all home strategies work for all parents. We adapt and partner with parents to determine next steps.
We think of success, not in number of bites or reducing the number of refusals, though that is one way to define progress. Instead, we look at the development of life-long skills, such as demonstration of a positive tilt, opening the mouth to indicate readiness for the offered spoonful or nipple with the child pacing the meal rather than the adult. We look at the life-long skill of confidently learning new food trying skills. We look at being able to eat with the family at a family meal. We look at positive food interactions (being able to touch food and pass food, serve food, help in mealtime jobs). We look at how many ways can the child feel celebrated around food and meals, (rather than feeling like he is disappointing his grownups every meal). Success can be the child bringing her own spoon to her mouth to feed herself rather than being fed by an adult. Success is also helping the child feel better, take in the needed nourishment, learn the skills to confidently chew and swallow foods and liquid, and enjoy the sensations of eating, and enjoy the mealtime with others. Can it be a success if a child can happily come to the mealtime, enjoy the food offered, and be allowed to leave the table when full?
The webinar I did for Feeding Matters is about how Food is Sensory. I outline lots of ways to look specifically at the look, smell, sound texture and taste of foods so we can carefully offer new foods in ways that dilute the worry and allow children to be active and joyful participants in the process.
- What can parents and healthcare professionals do to create an environment that encourages positive mealtime experiences?
The first thing I like to do is help parents and professionals imagine THEY ARE THE CHILD who is struggling to eat. Imagine how THEY themselves would like to be approached if THEY had a big mealtime worry, if they were worried about texture, or swallow safety, or if they felt badly when they ate, or if they could not manage the skill of eating. I have always thought that putting myself in someone else’s shoes is a great starting place. (Check out the Grasshopper Story ).
The second thing I think about to encourage success is starting from a place of MEALTIME PEACE. When parents and children are totally stressed about mealtimes, it is hard to help either of them want to try anything new. I ask parents, what would YOU need to do in YOUR house to achieve Mealtime Peace, a mealtime with no anger, crying, pushing, arguments, and no pressure? Maybe the child needs rehearsals, to learn how and what others eat. Maybe she needs food rehearsals where she gets to explore the food before well-meaning grown up puts it in her mouth. Maybe the child needs to be offered new foods or textures in such tiny incremental sensory changes so that it is hard for her to notice (or worry ) about the change? Maybe the child needs to eat comfortable foods at the meal and work on new food trying away from the meal, bringing the new food or skill to the table when comfortable? We aim for Mealtime Peace because when calm and comfortable, children are in more of a learning mindset rather than an escaping mindset. They can learn about family togetherness, manners and what to expect from a meal. They can trust at that place of Mealtime Peace that they will not be forced or pressured into trying new, that there will not be sensory surprises and that they are a celebrated part of the meal.
- What tips do you have for families and healthcare professionals looking to introduce new foods to a child with a pediatric feeding disorder?
When introducing new foods, can we start with foods or liquids that the child enjoys or is currently successful with? Success, comfort and enjoyment can be our starting place.
I like to offer rehearsals in trying new foods. In a rehearsal, a child gets to see others eating and interacting with that food. They get to see what we do with that food and how we eat it. They get to explore the look, smell, sound, texture and taste of the food before it ends up in their mouth. No sensory surprises. They get to help put it in their own mouth, or to their own lips when THEY are ready, when the rehearsal was motivating and they show interest or readiness. Sensory exploration of the foods helps the child be ready for it. For example, smelling a food is a rehearsal or preview that gives the child an idea about the taste before it is put in her mouth. Touching the food can give the child the idea of the food texture, again, before it is on her tongue. If you were worried about trying a new food, would you put a food in your mouth that you could not, would not even touch? Having these sensory rehearsals can really help.
- Considering the newly published consensus definition of PFD, which domain or factor do you feel most greatly influences the child’s relationship to food and the caregiver who feeds them?
In my experience, all the domains of PFD, medical, nutritional, feeding skills and psychosocial, influence the child’s relationship with foods and their caregiver. When a child struggles to eat for any reason, caregivers worry. Infants and children communicate that their mealtimes are not working for them by not eating, not eating enough, struggling with the motor skills of eating and sensory aspects of foods and, often, pushing their caregiver away. These reactions influence their relationships with food and with those who lovingly want them to eat more or differently.
As parents and professionals try to understand the roadblocks to confident and enjoyable eating, the mealtime interactions can become a stressed communication. The medical aspects of PFD relate to how well the child feels, if they have the endurance and physical abilities to eat. The nutritional aspects relate to the child’s ability to take in enough nutrition on their own to grow well. The feeding skills including muscle, motor coordination and sensory aspects of food influence eating enjoyment and confidence. And the psychosocial aspects of eating relate to the child’s interactions with caregivers and the mealtime. The meal becomes a constant dialogue where the child communicates her abilities and enjoyment and the caregivers listen and adapt to help make the mealtime successful and enjoyable. So, PFD is all of those domains. It is difficult to look at only one when helping children learn to enjoy foods and eat enough.
- It seems that enjoyment of a mealtime is very individualized. What role might more protocol based approaches have in the treatment of PFD?
I think enjoyment, confidence and internal motivation are big goals in supporting children who struggle with eating.
I personally like the word, “guideline” rather than “protocol”. I have almost five decades of experience with a more “guideline” approach that is responsive to the child’s reaction. We offer. The child is able to take that food, or not. If yes, GREAT. If no, we adapt the presentation for success to grade our ask. Was the texture, the bite size, the wetness of the texture too much? Can we adapt for success? When relying on protocols, or teaching protocols to parents, I have found that it can sometimes lead to stricter, less flexible and less individualized interpretations and approach. I have listened to parents my whole career, and many tell me when they were sent home with a protocol, it did not feel natural and was harder for them to implement in the home. We can all contribute. I believe there are many, many ways to support children who struggle to eat and that parent find the approaches that work for them.
About Marsha
Marsha Dunn Klein OTR/L,MEd, FAOTA is a pediatric occupational therapist who has spent a career specializing in pediatric feeding challenges. She received her bachelor’s degree in occupational therapy from Sargent College of Boston University in 1971. She also received a master’s degree in education with emphasis on special education in 1975 from the University of Arizona. Marsha has co-authored PreFeeding Skills editions one and two and Mealtime Participation Guide and Homemade Blended Formula Handbook with Suzanne Evans Morris and Feeding and Nutrition for the Child with Special Needs with Tracy Delaney. Marsha’s new book Anxious Eaters, Anxious Mealtimes: Practical and Compassionate Strategies for Mealtime Peace serves as a great resource for parents and caregivers. She lives in Tucson, Arizona and travels to present locally, nationally and internationally on pediatric feeding issues.
If you haven’t had a chance to watch Marsha’s virtual workshop “Food is Sensory,” you are welcome to participate on demand. It will be available on demand through April, 2020.
PFDA Quarterly Update
Published by Feeding Matters on Oct 10, 2019
-
- A PowerPoint Presentation on PFD has been drafted and will be piloted with our university partners from all four domains as we work to educate upcoming practitioners on PFD.
- The first completely virtual International Pediatric Feeding Disorder Conference agenda has been established and is now open for registration.
- Our educational resources, including products, texts, articles, and handouts are under construction and expanding. Criteria for resource review and inclusion has been developed to ensure resources are relevant, evidenced based and aligned with our mission.
-
- A proposal has been finalized and submitted to the CDC advocating for PFD to be a standalone diagnosis.
- Early intervention eligibility standards are under investigation as we build a better understanding of each state’s EI service model.
- We have identified the need for a consensus on assessment and management of PFD. Resources continue to be gathered as we prepare for a formal consensus meeting.
-
- The prevalence study on PFD is complete and has been submitted for peer review.
- The research blueprint has been finalized. View the Theory of Change to see what is next on the research agenda.
 Participate in the Alliance https://www.feedingmatters.org/pfd-alliance/advocacy/
Participate in the Alliance https://www.feedingmatters.org/pfd-alliance/advocacy/
 Contribute knowledge https://www.feedingmatters.org/get-involved/volunteer/become-a-volunteer/
Contribute knowledge https://www.feedingmatters.org/get-involved/volunteer/become-a-volunteer/
 Leverage resources https://www.feedingmatters.org/resources-support/resource-library/
Leverage resources https://www.feedingmatters.org/resources-support/resource-library/
 Support families https://www.feedingmatters.org/get-involved/give/
Support families https://www.feedingmatters.org/get-involved/give/ 
Introducing LACI: Learning Advanced through Collaborative Initiatives
Published by Feeding Matters on Sep 06, 2019
- Therapists will be able to utilize a local network for collaboration and expertise/advice.
- Referrals to the proper healthcare provider will be made more accurately and effectively, thereby decreasing waitlists for medically fragile children.
- Enhanced collaboration through a highly skilled cohort of medical professionals will enable enhanced care.
- Licensed OTR or SLP in good standing
- Currently or previously employed in a pediatric setting
- Strong commitment to professional growth and community partnering
- Statement of commitment: minimum of 4 hours per month to be allocated to collaborative goals
- Attend an in-person LACI launch meeting on October 22, 2019 and LACI conclusion meeting on April 21, 2020 from 4-6pm.
- Attend monthly 1-2-hour virtual LACI meetings for the 6-month cohort period: meetings to be held November 2019-March 2020.
- Engage in at least 2 hours of person-to-person collaboration or self-directed learning
- Contribute related resources and insight on the curriculum topic monthly via the virtual platform
- Complete feedback surveys as applicable
Open Call for Abstracts: PFD Research Small Grant Program
Published by Feeding Matters on Sep 02, 2019
- Scientific Reviews – such as systematic, meta-analysis, or scoping; addressing assessment, management, and/or treatment approaches for domains of PFD: medical, nutrition, feeding skill, and psychosocial. The following list offers review suggestions:
- Assessments used in the PFD field (tools, clinician assessments, and/or tests)
- Therapeutic outcomes and/or approaches for PFD treatment
- Resource utilization or economic studies – cost of PFD from the perspective of the healthcare system and/or the family.
Please consider applying using the information below…
General Guidelines and Eligibility:- Funding up to $5,000 for one year from date of award
- No indirect costs or overhead costs
- United States residents
- Methodology must follow PRISMA guidelines
- Open call for abstracts – Friday, September 27, 2019 (by 11:59pm Pacific Time) *new deadline*
- All dates subject to change due to open call deadline extension
- Request for full proposals to be sent to applicants– Wednesday, October 16, 2019
- Full proposal application due – Friday, December 6, 2019 (by 11:59pm Pacific Time)
- Funding and projects begin – Early 2020
- Contact information (name, email, phone number, and mailing address)
- Qualifications & credentials
- Supervising academic mentor (if applicable)
- Funding priority requesting
- Abstract (400-600 words)
- Background
- Research question
- Methodology
- Timeline
For additional information and guidelines, please download the funding guidelines below.
Infant Allergy Awareness Month
Published by Feeding Matters on Jul 18, 2019
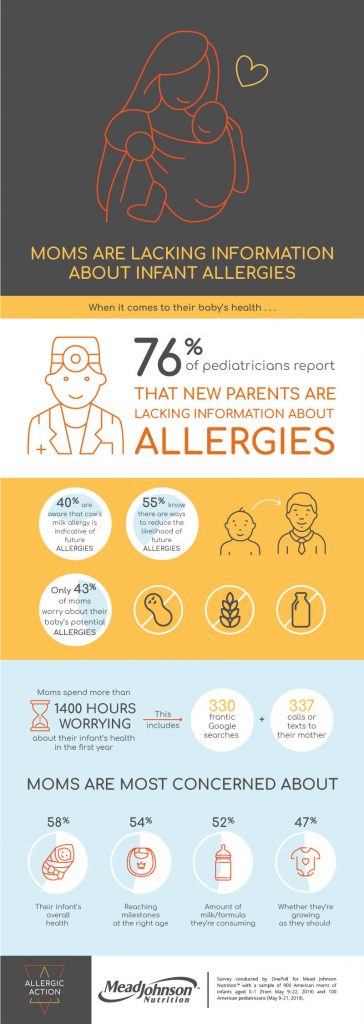 Food allergies in infants and children are becoming more prevalent. A new survey of 900 US moms (of children aged 0-1) and 100 US pediatricians took a look at the issue.
WHEN IT COMES TO THEIR INFANTS’ HEALTH, MOMS ARE WORRIED ABOUT . . .
58% – Their overall health
54% – If they’re reaching milestones at the right age
52% – The amount of milk/formula and/or food they’re consuming
47% – If they’re growing as they should
47% – Their nutritional intake (e.g. vitamins, supplements)
43% – If they have any allergies
41% – The amount of sleep they’re getting
40% – If I’m bonding enough with them
36% – The quality of sleep they’re getting
36% – What their different cries meant
HEALTH ISSUES MOMS HAVE EXPERIENCED IN THEIR INFANTS
54% – Diaper rash
41% – Fever
36% – Cradle cap
34% – Baby acne
32% – Vomiting
30% – Issues breastfeeding
25% – Ear infection
23% – Colic
21% – Allergies
11% – Swollen belly
With 76% of pediatricians reporting that new parents are lacking information about allergies, it’s necessary to stay up-to-date on current treatment and diagnosis information. Health care professionals can learn about the symptoms, diagnoses, and management of food allergies at PNCE.org/food-allergies.
Food allergies in infants and children are becoming more prevalent. A new survey of 900 US moms (of children aged 0-1) and 100 US pediatricians took a look at the issue.
WHEN IT COMES TO THEIR INFANTS’ HEALTH, MOMS ARE WORRIED ABOUT . . .
58% – Their overall health
54% – If they’re reaching milestones at the right age
52% – The amount of milk/formula and/or food they’re consuming
47% – If they’re growing as they should
47% – Their nutritional intake (e.g. vitamins, supplements)
43% – If they have any allergies
41% – The amount of sleep they’re getting
40% – If I’m bonding enough with them
36% – The quality of sleep they’re getting
36% – What their different cries meant
HEALTH ISSUES MOMS HAVE EXPERIENCED IN THEIR INFANTS
54% – Diaper rash
41% – Fever
36% – Cradle cap
34% – Baby acne
32% – Vomiting
30% – Issues breastfeeding
25% – Ear infection
23% – Colic
21% – Allergies
11% – Swollen belly
With 76% of pediatricians reporting that new parents are lacking information about allergies, it’s necessary to stay up-to-date on current treatment and diagnosis information. Health care professionals can learn about the symptoms, diagnoses, and management of food allergies at PNCE.org/food-allergies. 
Register Now: 2019 Virtual Town Halls
Published by Feeding Matters on May 21, 2019
 Kate Barlow, OTD is an Assistant Professor of occupational therapy at American International College and a feeding consultant for THOM early intervention. She is also the current ambassador for the CDC’s Learn the Signs. Act Early. Program for the state of Massachusetts. She has over 20 years of clinical practice and her area of expertise is feeding, eating and swallowing.
Kate Barlow, OTD is an Assistant Professor of occupational therapy at American International College and a feeding consultant for THOM early intervention. She is also the current ambassador for the CDC’s Learn the Signs. Act Early. Program for the state of Massachusetts. She has over 20 years of clinical practice and her area of expertise is feeding, eating and swallowing.