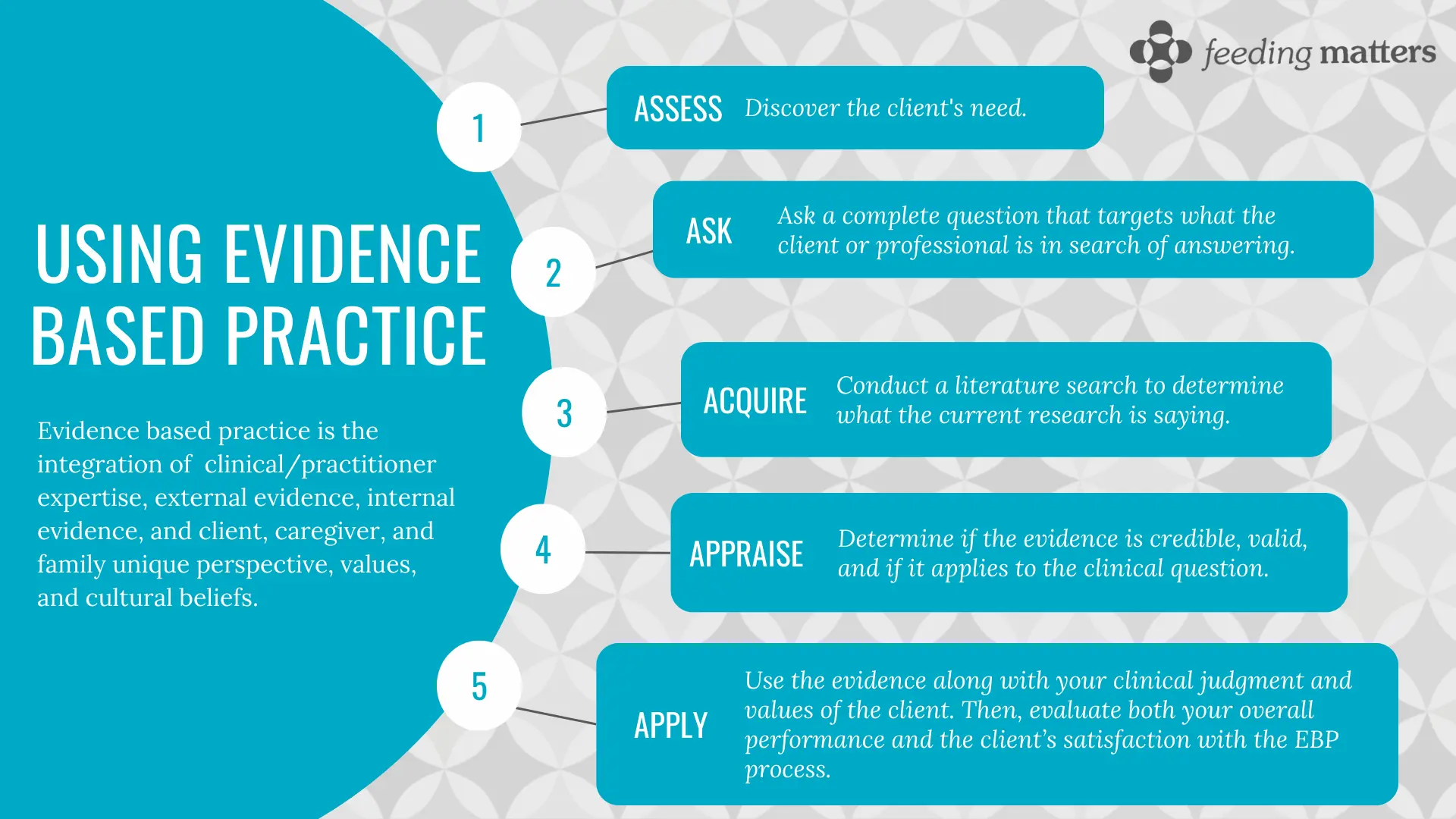
What is evidence-based practice (EBP)?
Evidence based practice is the integration of clinical/practitioner expertise, external evidence, internal evidence, and client, caregiver, and family unique perspective, values, and cultural beliefs.
Clinical/practitioner expertise
The knowledge, judgment, and critical reasoning acquired through a practitioner’s training and professional experiences.
External
The best available information gathered from the scientific literature.
Internal evidence
The data and observations collected on your individual client within a practitioner’s practice setting.
Client, caregiver, and family unique perspective
The unique set of personal and cultural circumstances, values, priorities, and expectations identified by your client and their caregivers.
 References:
References:
- ASHA (2023). Evidence-Based Practice. https://www.asha.org/research/ebp/
- UNC (2022). Rehabilitation service line resources: UNC hospitals: Evidence-based practice. https://guides.lib.unc.edu/rehabilitation-line/evidence-based
2023 Study
This 2023 mixed-method study by Dr. Paula Rabaey and Dr. Kate Barlow sough to identify which assessment tools were utilized by feeding skill providers (occupational therapists and speech-language pathologists) to diagnose PFD. The study revealed the lack of a standardized approach to PFD assessment and continued reliance on non-standardized assessment tools. Currently, available assessment tools do not comprehensively assess all four domains of PFD which calls for a broader and more formalized manner to assess the complexity of PFD. Read the study.
Paula A. Rabaey, Kate Barlow, Hibak Jama, Victoria Lehr; Investigation of Assessment Tools in the Area of Pediatric Feeding Evaluation: A Mixed-Methods Study. Am J Occup Ther July/August 2023, Vol. 77(4), 7704205110. doi: https://doi.org/10.5014/ajot.2023.050040
Supporting Family Advocacy for Evidence-Based Practice
What can families do?
- Ask questions. You have a right to understand your child’s care and your care options. Ask why a treatment was recommended and if there are any risks.
- Request information in a form you understand. Ask for information in writing, in picture form and in the language you prefer.
- Share what matters most to your family. It is important that your provider know what you value and what is important to you and your family.
- Ask for the evidence and ask how well researched the evidence is. Not all evidence is created equal. Request a conversation with your provider to discuss the evidence together.
- Share what is happening at home. Your provider needs to understand your daily life and your current needs to best help you and your child. Use videos, pictures, and your own story to share your life with PFD.
What can providers do?
- Create an environment conducive to open communication. Families need time and a safe space to share their thoughts. Work to establish trust before discussing treatment options with families.
- Champion collaboration: The family makes the decisions for their child’s care. Involve families in decision-making, care planning, and determining if a treatment has been a success by fostering collaboration continuously.
- Use the evidence to inform decision-making. Seek the best available evidence from research, family input, and utilize your clinical expertise when designing and implementing care plans with the family.
- Write family/child-centered goals and focus on family-centered outcomes. Outcomes should be relevant, valued and actionable to the family.
- Self-reflect. Engage in ongoing self-evaluation, ask for feedback from families and use shared feedback to make meaningful changes to how you deliver care.
EBP Resources by Domain
Medical
Nutrition
-
- Academy of Nutrition and Dietetics (2023). Evidence analysis library.
Feeding Skill
-
- American Occupational Therapy Association (2023). Practice essentials: Evidence-based practice and knowledge translation.
- ASHA (2023). Evidence-based practice.
Psychosocial
-
- American Psychological Association (2023). Evidence-based practice in psychology.