Category: Family Stories

Establishing a Self-Care Plan When Caring for a Child with Disabilities
Published by Dorothy Watson on May 04, 2023
This blog post was submitted by community member Dorothy Watson at mentalwellnesscenter.info. Interested in having your work on our blog? Learn more here.

Taking care of a child with disabilities can be incredibly rewarding, but it’s also incredibly challenging. The weight of responsibility and feeling of being overwhelmed can often lead to burnout for parents and caregivers. These individuals must make self-care an integral part of their plan to prevent burnout. This blog post will provide information and tips on how to create a sustainable self-care plan specifically designed for parents or caregivers of children with disabilities.
Learn To Recognize Triggers
The first step in creating an effective self-care plan is to identify triggers that cause stress, anxiety, or overwhelm. Identifying triggers allows individuals to recognize when they may be headed toward burnout and take steps to avoid it. For example, if going grocery shopping with your child causes high levels of stress, you can look for ways to make the experience easier or find alternatives such as ordering groceries online. Once you have identified your triggers, you can find ways to manage them proactively and prevent burnout from happening in the first place.
Assess Your Fatigue Levels
Caregivers should also become aware of their fatigue levels to create a successful self-care plan. When caring for someone who is on the autism spectrum, energy management becomes even more important as it can be easy to get burned out quickly due to constantly dealing with new challenges and trying different approaches.
Developing awareness around your energy levels will allow you to adjust your self-care plan accordingly when needed and create realistic expectations so that you don’t become overwhelmed by the tasks ahead of you. Sometimes, small changes like reducing clutter and spending more time in nature can be the boost that you need to get through the day. Both have been shown to reduce stress and life moods.
From Architectural Digest Reviews
According to a recent survey, around 33% of people report feeling extreme stress. Promoting a stress-free home environment has been linked to better physical and mental health. A peaceful home not only aids in sleep, reduces stress, and enhances overall well-being, but also boosts productivity and can help us find relief from the demands of daily life.
Our team believes that homeowners should feel at peace in their homes amidst their busy and hectic lives. We published a piece that includes ways to de-stress your home without sacrificing your style or time. Our team believes that homeowners should feel at peace in their homes amidst their busy and hectic lives. We published a piece that includes ways to de-stress your home without sacrificing your style or time.
Set A Few Personal Goals
Another important step in creating a sustainable self-care plan is setting realistic personal goals that are achievable within any given timeframe. Goals such as returning to school or finding a new job may seem out of reach at times, but utilizing tools like an online resume builder can be especially helpful in this process.
If you’re not sure where to get started, look for websites that allow you to choose a free professional template and add your own custom touches, such as an eye-catching font. If your goal is to start a business, look for help with forming an LLC for protection; a formation service can handle the paperwork so you can ensure your business receives all the tax benefits that come with it.
Utilize Self-Care Tactics
Once realistic goals have been established, utilizing various self-care strategies is crucial in avoiding burnout while taking care of someone with special needs. Try mindfulness practices like yoga or meditation, spending quality time with friends or family members, taking regular breaks throughout the day, getting enough sleep each night, and engaging in leisure activities that bring joy. These strategies allow individuals caring for someone who is on the autism spectrum time away from their responsibilities while still feeling capable and productive enough themselves.
Take Care of Your Body
When you care for someone else, it is easy to put your own needs lower on the priority list. But that is a big mistake. When you don’t care for your body, you actually become more tired and unmotivated. Instead, take steps to treat your body like it deserves to be treated. Fill your kitchen with healthy snacks, like fruits and nuts, that you can grab instead of something sugar-laden. And make an effort to park farther from your destinations so that you can get in a few more steps. You’ll find yourself feeling better physically and mentally more quickly than you might expect.
These practices will also help your little one to see what it looks like to be healthy. If you struggle getting your child to eat healthy foods, modeling is one great way to help change their perspective on those foods. You can also reach out to Feeding Matters, especially if you feel that your child may have pediatric feeding disorder. They have resources to help you help your child with their eating habits.
Ask For Help When You Need It
Although creating an effective self-care plan is essential when caring for a child with disabilities, it’s also important to seek professional assistance when needed so that burnout doesn’t take over entirely. There are counselors available both online and offline who specialize in helping individuals cope with life transitions associated with taking care of someone who has special needs. Additionally, there may be local support groups available where caregivers can come together and share stories and experiences, and this can help you figure out a care plan.
Consider Everyone’s Needs and Make a Plan
Creating an effective self-care plan as a caregiver for a child with disabilities can take some time, as you’ll need to constantly assess what works and what doesn’t. Consider keeping a journal that will help you vent your frustrations, and look for online resources that will assist with goals like starting an LLC or finding a new job. Try to be patient as you get started and know that once you begin to find strategies that work, the pieces will fall into place.
The views and opinions expressed in this blog post are solely those of the author who submitted it and do not necessarily reflect the views of Feeding Matters. We do not endorse any products or services mentioned in the post, and we are not responsible for any errors or omissions in the content. The information in this post is provided for educational and informational purposes only, and should not be considered as a substitute for professional advice.
The Power of Trauma Informed Care for Children with Pediatric Feeding Disorders
Published by Feeding Matters on Apr 05, 2023
Of all the clinical appointments for 15-year-old Maya Roberto over the years, one stands out. Instead of catatonically going through the motions of her echocardiogram, Maya interacted with her cardiologist, even asking questions. Her mother, Dr. Anka Roberto, recalls how shocked she and her doctor were as Maya actively engaged with her cardiologist for the first time.
Noting that his patient, who was five years old at the time, was much more lively, the physician asked what had changed. Roberto, DNP, MPH, APRN, PMHNP-BC told him, she was in trauma therapy and just had an Eye Movement Desensitization and Reprocessing (EMDR) session to help her work through her medical trauma.
The doctor had never heard of it, and was pleasantly surprised with its efficacy.
Today, Roberto uses EMDR to help heal her pediatric patients from trauma as a private practice clinician.
Roberto’s years as a NICU nurse and mother of a child with complex congenital heart defects prepared her for a career in trauma-informed care as an advanced practice nurse. She’s seen personally and professionally how much treating a patient’s trauma as part of the continuum of care can make a difference.

Since birth, Maya’s journey has included multiple open heart surgeries, years of feeding therapy and an NG tube. Roberto knows firsthand how traumatic medical and feeding interventions can have a lasting impact. For children with pediatric feeding disorder (PFD), considering and treating medical trauma can go a long way toward healing children.
Trauma-informed care offers a comprehensive approach that considers emotional and mental well-being to help children and their families affected by PFD. Understanding the impact of trauma on the body and how to navigate it allows families to access an effective care modality.
Defining trauma
Trauma varies for everyone. One major incident or many minor insults can cause trauma. Two people experiencing the same situation can respond entirely differently. One can move forward, while the other carries a lasting physical and emotional imprint. “When I think about trauma, it’s more of an adversity,” says Roberto. “We could have a big trauma, or we can have little things that add up to carry the same weight of a big trauma.”
What matters is how trauma affects the brain and body.
The CDC-Kaiser Permanente Adverse Childhood Experiences (ACE) study is one of the most comprehensive investigations into the lasting effects of childhood trauma. The longitudinal study showed that early adversity could significantly impact future physical, social and emotional health – as well as lead to early mortality rates.
The pandemic further raised awareness of how trauma can affect mental and physical health.
How the body reacts to trauma
Trauma can profoundly affect the body. Potentially traumatic experiences trigger the body’s “fight or flight” response. In this state, the heart rate increases, and respiration speeds up as the sympathetic nervous system prepares to defend against danger.
The disruption of hormones and enzymes caused by the experience can lead to difficulty regulating temperature, breathing and digestion. The gastric emptying system turns off. It causes constipation, loss of appetite, and/or motility (muscles in the wall of the gut) issues.
“It’s like the fire alarm in the house is going off,” says Roberto. When this happens, the parasympathetic system, sometimes called the “rest and digest” system, stops working.
These acute responses can make an imprint that has long-term effects. Families of children with PFD can mitigate the impact of trauma with support and care. “Trauma leaves a mark, but it’s up to us to find those who can help us get out of being stuck in the triggered cycle,” says Roberto
Understanding trauma-informed care for children with PFD
Trauma-informed care is an approach to support those who have had adverse experiences during their lifetime. Unlike traditional forms of care, which may not be sensitive to traumatic experiences, trauma-informed care recognizes the impact of trauma on an individual’s behavior, thoughts and emotions. The goal is to create a safe space for healing and recovery.Trauma-informed care involves four key components, known as the “Four R’s:
- Realizing how trauma can affect an individual
- Recognizing signs an individual has experienced trauma
- Responding effectively with appropriate interventions
- Resisting re-traumatization by promoting safety, trust, empowerment and collaboration
Understanding these components is essential to effectively support children with PFD, who may be dealing with the long-term effects of traumatic experiences.
Trauma can disrupt eating patterns by causing fear or anxiety around food, leading to refusal or avoidance behaviors. This compounds feeding issues children with PFD already experience.
For children with PFD, trauma-informed care offers a safe way to explore emotions while helping them build positive relationships around eating.
How to navigate the impact of feeding trauma
The effects of trauma on children with PFD can be challenging. What’s traumatic to one child may barely register for another. And the traumatic experience often isn’t even something the child can recall.
This is why it’s crucial to understand each child’s experience, recognize triggers and provide emotional support. Therapeutic interventions such as EMDR can help children reprocess past traumas without needing to talk about them. In her practice, Roberto uses a sand tray and play therapy to help children process previous experiences and feelings.
“They may not have verbal recall and a story to tell, but they remember feeling a certain way,” she says.
A child’s visit to a doctor’s office, for example, can trigger a panic attack because they don’t want to lie on the table, says Roberto. “It’s really because of this unprocessed adversity, which for many people may come from a place of not having control.”
With EMDR, she helps children uncouple the emotional tenacity from that memory.
Benefits of trauma-informed care for children with PFD
Trauma-informed care provides a safe space for families to build trust and better understand how to support their children. Trauma-informed care allows children to explore the experiences that triggered their trauma and develop improved emotional regulation skills. It can also lead to an improved appetite and a willingness to try new foods.
When children get emotional support, they can better articulate their needs to their parents and healthcare team. A therapist can help a child develop practical communication skills and problem-solving techniques. With practice and guidance, these tools allow children facing medical trauma to cope more effectively in difficult situations.
3 ways to support children with feeding trauma
Finding the right resources for trauma-informed care can be challenging, but more resources are developing with a heightened awareness of trauma’s impact.
Focus on the whole family
Roberto says supporting the entire family is key to helping children heal from traumatic events. “Families are like a tree, so if one limb is struggling, the others will start to wither as well.”
Give kids time
Children with medical complications react to stress in the same instinctual way as anyone who senses physical danger. Anyone who’s had to submit their child to medical testing has likely witnessed the fight, flight or freeze response. Roberto recommends slowing down in those moments. “Listen to your kids and give them the time to get there. It’s not about our agenda, as parents or as clinicians. It needs to be about the child’s agenda and providing them with the support they need in the moment.”
Get outside support
Talk to your child’s doctor or pediatrician about what type of care is available in your area and look for mental health providers who specialize in this trauma-informed therapy.
Online resources can also be helpful when seeking out trauma-informed care. The National Child Traumatic Stress Network offers comprehensive information geared toward helping families affected by traumatic events.
Finally, it’s important to remember that although trauma can be difficult, it can be an opportunity to move forward and break the trigger cycle. Roberto says, “We all have our experiences, but we don’t have to let them define us or limit our future possibilities.”
By understanding the trauma children with PFD can experience and working through it with compassion, children can regain control over their lives and reach their full potential.
Anka Roberto, DNP, MPH, APRN, PMHNP-BC an assistant professor at the University of North Carolina Wilmington and has authored book chapters and numerous publications on trauma and resilience. In her private practice, Holistic Healing, PLLC, she provides functional psychiatry care and EMDR therapy to target and reprocess negative life experiences across the lifespan.
Roberto is the keynote speaker at the 10th Annual International PFD Conference on April 13-14. Click here to learn more and register.

What I learned working with a pediatric dietitian
Published by Jalenna Francois on Mar 29, 2023
March is National Nutrition Month! Read along to meet Feeding Matters staff member Jalenna Francois and her experience working with a pediatric dietitian.
 Hi! My name is Jalenna Francois. I am the Communications and Awareness Specialist at Feeding Matters. My daughter Sophie was born two years ago (this Friday is her birthday — happy birthday, Soph!). We struggled with feeding pretty immediately after she was born. With the help of a tongue and lip tie revision, lactation consultant, osteopathic manipulation, and the removal of milk from Sophie’s diet, we made huge improvements. I am forever grateful for the early intervention Sophie received, which occurred in part because I’ve worked for Feeding Matters for nearly ten years and know the early signs of a potential pediatric feeding disorder.
Hi! My name is Jalenna Francois. I am the Communications and Awareness Specialist at Feeding Matters. My daughter Sophie was born two years ago (this Friday is her birthday — happy birthday, Soph!). We struggled with feeding pretty immediately after she was born. With the help of a tongue and lip tie revision, lactation consultant, osteopathic manipulation, and the removal of milk from Sophie’s diet, we made huge improvements. I am forever grateful for the early intervention Sophie received, which occurred in part because I’ve worked for Feeding Matters for nearly ten years and know the early signs of a potential pediatric feeding disorder.
As she grew, we discovered she had IgE-Mediated food allergies (what you think of when you hear about food allergies, for Sophie they typically present as hives and wheezing) and FPIES (Food Protein Induced Enterocolitis Syndrome, which presents as vomiting several hours after ingestion of a trigger food). Both of these are comorbid conditions for pediatric feeding disorder.

Our family has been on a long feeding journey over the past two years, and it was changed forever because of our work with a pediatric dietitian. I have learned many lessons from these regular visits with Sophie’s dietitian:
- Nutrition is a lot more than what’s on our plates.
While I did learn about nutrients, how to pair foods, and substitutions to get Sophie what she needed from her limited diet, I also learned that there is a lot more that goes into feeding my family than how many servings of vegetables we get. I learned to acknowledge and set aside the cultural expectations, personal expectations, and the fear and anxiety which wasn’t helping us meet our needs. I learned to meet Sophie where she was with eating. - Meals carry a lot of emotion!
It is so easy to get overwhelmed, anxious, and stressed about feeding my family. Can (or will) Sophie safely eat this? Did she eat enough? Are we eating enough variety? Wow, allergic reactions are scary! As I began to recognize the power this anxiety held over me, I could see it trickling down to my kids as well. At the suggestion of our dietitian, we now check in on emotions before we sit down at the table. There are nights where we can jump right in to eating, but other nights, we need a family story time to connect, take off the pressure, and enjoy just being together before we eat. Creating this feeling of connection and safety before we get to the table has helped to reduce the immediate ‘YUCK’ my 4-year old likes to react with when she sees the foods being offered. - Lead by example.
For me, this has looked like taking intentional time to feed myself food that is nourishing and enjoyable. I don’t let my kids skip meals, and I am trying to treat myself the same way. I have learned to incorporate all foods I enjoy without guilt, in a balanced way. Caring for myself will only benefit my children as well. - Give yourself grace. Feeding is a journey, and progress is more important than perfection.
Not every meal is going to go perfectly, not every food is going to be accepted, even after 100 exposures. Having patience with myself and my children as we learn together is building the trust we all need to make progress. - The power of having someone in your corner.
Having someone to talk over meal plans and strategies for food introductions and substitutions was huge. But what I remember from the beginning of our journey with our dietitian was having someone to help me see hope when our feeding experiences felt overwhelming, never-ending, or unfair. Having someone who gets it and is able to help you see the possibilities ahead is a game changer. (Pro tip: Looking for someone to be in your corner? Check out the Feeding Matters Power of Two program.)
 By now, I’m sure you can tell that my dietitian is awesome! Not only is she a great dietitian, she shares her extensive knowledge on her Instagram and blog so that everyone can learn like I have. She also recently became a Feeding Matters board member, which is just one way she is as a champion for children with PFD.
By now, I’m sure you can tell that my dietitian is awesome! Not only is she a great dietitian, she shares her extensive knowledge on her Instagram and blog so that everyone can learn like I have. She also recently became a Feeding Matters board member, which is just one way she is as a champion for children with PFD.
As we celebrate Sophie’s second birthday this week, I am so proud of the progress our family has made together. I never imagined we would make it to where we are today, and I look forward to seeing where the rest of our journey takes us, with our dietitian by our side.

Does your child need a feeding tube? Here’s what you need to know
Published by Dana Williams, MD on Feb 09, 2023
A pediatric gastroenterologist debunks 4 myths about G-tubes and normalizes a feeding tube for those kids who need it.
 Dana Williams, MD, Medical Director, Feeding Disorders Multidisciplinary program; Medical Director, Aerodigestive Digestive Program at Phoenix Children’s Hospital
Dana Williams, MD, Medical Director, Feeding Disorders Multidisciplinary program; Medical Director, Aerodigestive Digestive Program at Phoenix Children’s Hospital
When I see patients who are likely candidates for a G-tube, I can already imagine their lives at home. Days revolve around feedings. Every hour, on the hour, the parents attempt to get an ounce of formula or breastmilk into their little one’s belly. The parents are exhausted, and so are their children. Everyone feels like a failure.
In spite of the struggle, no one wants to bring up a G-tube. So, I do.
As director of a team of physicians, therapists and dietitians at Phoenix Children’s Hospital, I see hundreds of children each year with pediatric feeding disorder (PFD). For many of them whose medical complexities make oral eating a struggle, a gastrostomy (G) tube is a key medical intervention. G-tubes help these children develop and thrive, while preventing malnutrition and dehydration.
A G-tube is surgically inserted through the abdominal wall and into the stomach. It’s held in place by an internal device called a balloon. The tube can be used to deliver liquids, purees and medication.
This sounds scarier than it is.
Like any surgical medical intervention, deciding to directly feed a child through a gastrointestinal tube inserted into their stomach is a big decision. For those children who are a good candidate for a G-tube, the benefits of a feeding tube and the risks of not getting one far outweigh any risks.
There are many benefits of getting a G-tube. Some of those include:
- Improved nutrition and hydration: A G-tube provides direct access to the stomach for nutrition, fluids and medication, ensuring children get the nutrition they need.
- Reduced risk of aspiration: A G-tube can reduce the risk of food and liquid entering the lungs, a common problem for children with pediatric feeding disorders.
- Increased independence: Children with G-tubes can engage in activities they enjoy without the stress of constantly worrying about eating or drinking.
- Better sleep: A G-tube can provide continuous nutrition and hydration overnight, leading to better sleep and improved overall health.
- Eased caregiver burden: Parents get relief from constantly trying to provide adequate nutrition and hydration.
- Improved weight gain and development: Children with a G-tube often see improved weight gain, leading to better overall health.
- Comfort: Removing the alternative temporary nasal tube can make it more comfortable for a child to eat. Depending on each child’s medical journey, they may be more likely to eat when they don’t have hardware in their noses.
Still, many parents who consider a G-tube for their children can feel like a failure. The truth is the opposite. Feeding isn’t something parents or doctors or anybody can control. If a child doesn’t want to eat, or they can’t eat, then there is nothing anyone can do to make them. Of course, this can change over time with multiple levels of support. But the parents of these children haven’t failed.
Debunking 4 major myths about G-tubes
Most of the time that parents express hesitation about the G-tube, it’s because of a fear of one or more of four common myths. Talking about the reality of what a G-tube will mean for a child and the family helps parents make an informed decision.
Myth #1: A G-tube is permanent
A G-tube is a temporary solution to supplement or replace oral eating and drinking. I have countless patients living healthy lives after the removal of their G-tubes who will attest to that fact.
How long each patient needs a G-tube and whether they’re receiving all or some nutrition through the tube depends on each child’s needs. When a family is deciding about G-tube surgery, we discuss the anticipated use. In many cases, a G-tube can supplement – rather than replace – oral eating.
We also discuss the process for removing a G-tube for those kids who can eat fully orally one day.
Myth #2: Infection is common with a G-tube
Infections do occur for some people with a G-tube, but they’re not common. Some children are more sensitive, and there is no way to predict that. For most people, the channel for the G-tube heals nicely. Similarly to an ear piercing, it becomes epithelialized so that the tube can comfortably pass through the area. We monitor the insertion hole and mitigate the risk of infection by teaching parents and older children how to clean the area.
Myth #3: Kids can’t eat regular food with a G-tube
The majority of kids with G-tubes in our practice also eat orally. This varies for each child, depending on their medical issues. Most children I see even take pleasure in oral food. The G-tube is an important tool that gives children time to develop the ability to eat on their own terms.
Myth #4: A G-tube means kids won’t be motivated to eat orally
While there is some truth to this myth, it’s not entirely accurate. For many kids with PFD, it doesn’t take much for them to feel full. This is why we individualize treatment so that each child receives the amount they need. Children can still learn hunger cues and get exposed to meal time routines.
What is a sign of success for a child with a feeding tube?
Just as the treatment plan for every child with a feeding tube is different, success also varies. To me, the main signifier of success is when the patient and family are in close conversation with their doctor. Every journey is different, but having a team of the right medical provider matters. It’s not up to parents to walk this journey alone.
Beyond that, any step forward for a child is success. Some examples are as follows:
- A child who aspirates due to a medical condition safely learns to taste some food and enjoy family meals.
- A child slowly learns to eat orally through feeding therapy post heart surgery.
- A child who outgrows some allergies and tries more foods.
- A young adult who goes off to college even though he still only eats seven foods.
Parents of children with pediatric feeding disorder no doubt feel responsible for ensuring their children get the nutrition they need to grow and develop. For those children who are good candidates for a feeding tube, a G-tube is an important tool to help them along their feeding journey.
Hadyn Van der Molen has had a G-tube since he was nine months old. His mom, Heidi, program manager for Feeding Matters, recalls feeding Hadyn around the clock with a 2-oz. bottle. The only time he’d ingest it was when he was sleeping.


Stressful Mealtimes and Misbehavior
Published by Cuyler Romeo, MOT, OTR/L, SCFES, IBCLC on Jan 31, 2023
Imagine sitting your infant down in the highchair for the first time to try solids. As you film the moment, your baby puckers his lips, spits out the puree and turns his head. Mealtime doesn’t improve with time. Instead, food refusal becomes more intense with every meal.
While your friends’ children are happily gumming puffed kale at the park, you can’t imagine offering food in public. You feel exhausted and isolated.
If your family has experienced difficult mealtimes, you’re not alone. I have been honored to support hundreds of families on their PFD journey as an occupational therapist and feeding specialist. Yes, for some children food refusal is a naturally occurring developmental stage, but for others it’s a sign of pediatric feeding disorder (PFD).
Mealtime Behavior Is Communication
All behavior is communication. Children’s communication skills develop over time, and many children are not fully equipped to manage intense emotions mealtimes can evoke. A child may use actions such as leaving the table or display strong emotions such as crying and screaming when their first attempts at communication aren’t heard.
Miscommunication and misinterpretation of communication behaviors can be exhausting for both the parent and the child. Mealtime stress signs may look like:
- Pursed lips
- Head turning
- Throwing food
- Leaving the table
- Gagging
- Retching
- Vomiting
- Screaming
- Tantruming
- Hitting
Causes of stressful behaviors at mealtime
While mealtime behaviors may look similar to families who are struggling to nourish their child, the reasoning behind the communication can vary. Children don’t want to eat and are afraid to eat for many reasons. Some conditions that can cause mealtime stress include the following:
- Food allergies
- Constipation
- Sensory sensitivities
- A structural or anatomical issue in the gastrointestinal tract or esophagus
- Alternate interpretations of food and food properties
- Medical complications in the lungs, heart or brain
- Pediatric feeding disorder (PFD)
Siblings of children with mealtime stress also may be impacted. Research shows that families with one child who struggles during meals are more likely to have multiple children who do.
How to improve your child’s behavior during meals
The underlying reason for your child’s stress behaviors during meals will help you determine your next steps. For example, if your child has a developmental delay or is neurodivergent, they may have more difficulty communicating their needs. They may need support to communicate without extreme stress.
Children who have a physical condition impeding their ability to eat may need support addressing the physical issue before they feel confident eating new or more complex foods.
Whatever the etiology (cause), it’s important to first ask, “What is my child communicating?” Acknowledge their feelings. Never force your child to eat. Seek support. Speak with your child’s pediatrician and share your concerns. Children who are struggling to eat can and do make progress with proper support.
Get help for stressful mealtimes and behavior concerns
Children learn to eat over time. As they grow and develop, their bodies support new feeding and eating skills. By the time a child is five, they will have mastered most oral-motor skills needed to eat a varied and textured diet. But the adventure of learning to eat new foods never ends.
Negative mealtime behaviors during these developmental years can be devastating to any family. Mealtimes should be positive, safe and enjoyable. If you dread mealtimes, this compounding stress can impact other areas of your parent-child relationship. In extreme cases, it can impact every interaction.
It doesn’t have to be this way.
Talk to your doctor if you’re feeling stressed about feeding or are concerned your child is not getting good nutrition.
Prepare for this conversation by taking Feeding Matter’s Infant and Child Feeding Questionnaire© (ICFQ) and print out or email the results to your pediatrician. This educational tool highlights red flags and builds a more concrete picture of your child’s feeding behaviors.
You may also find it helpful to bring a mealtime record of what, when and how your child eats. A short mealtime video also can be useful to share with your pediatrician.
Your doctor can help rule out medical complications and connect you with other professionals, such as occupational therapists and speech language pathologists with specialized training in feeding. These professionals will help you develop and embed new strategies and behaviors into your family’s daily routines.
The skills needed for safe and pleasurable mealtimes take time to develop. Your therapist should partner with you to identify strategies that will be safe and successful for your child.
Click here to take Feeding Matter’s ICFQ. Find a feeding specialist in your area by visiting Feeding Matters’ Provider Directory. Cuyler Romeo is Director of Strategic Initiatives at Feeding Matters and a clinician at Banner-University Medical Center’s NICU.
Picky Eating: Just a phase or cause for greater concern?
Published by Cuyler Romeo, M.O.T., OTR/L, SCFES, IBCLC on Jan 30, 2023
How to know if your child will outgrow picky eating. Plus, how to survive mealtimes with the pickiest palates.
From birth, the majority of time you spend with your infants and young children revolves around food. Children eat a minimum of six times a day. It takes hours to prepare food, feed kids and clean up.
This means that when feeding becomes a challenge, parents can feel like a failure. That was the case for Natalie Peterson, mom of Easton.
When Natalie introduced Easton to solid foods at 4.5 months, she immediately knew something was off. “How he reacted felt different. I brushed it off initially but I think deep down in my gut, that mom instinct knew something was different.”
They tried again and ran into that same reaction. Easton pushed the food away, refused it and even became angry. “It was incredibly isolating. It felt like we had failed him.”
Easton was the first child in the U.S. to be diagnosed with pediatric feeding disorder (PFD).
And Natalie certainly wasn’t the only parent to feel anxiety, frustration and shame over picky eating.
How common is picky eating?
Picky eating is a common disorder during childhood. According to Dr. Kay Toomey, pediatric psychologist and member of Feeding Matters, a variety of studies across the world suggest that approximately one-fourth to one-third of children on average will struggle with some type of feeding and/or growth issue in their first decade.
Picky eating can look similar, but the causes vary. Many toddlers experience a phase of picky eating when they need fewer calories than during months when they were growing faster. That decrease in appetite coupled with their curiosity about boundaries can lead to fussy eating.
It’s when this persists or becomes more extreme that picky eating could be a sign of another underlying condition, such as pediatric feeding disorder (PFD).
What is considered picky eating?

According to Dr. Toomey, the operational definition of picky eating is children who demonstrate either transient or more extended challenges (up to 2 years duration). She outlined the following feeding and eating patterns in a presentation for Feeding Matters:
- Strong preferences
- Limited variety
- A restricted number of foods they will eat.
- Avoiding new foods
- Refusing the “right” foods or the “right” amounts
- Getting more upset than peers
- Requiring a special meal by their parents
- May eat differently in different contexts
How can I help my child with picky eating?
While many children will be picky eaters in spite of parents’ best efforts, there are a few ways to encourage children to eat better.
Following are a few ideas you can try if you’re experiencing stressful mealtimes:
Establish a mealtime routine. Children find comfort and confidence in a predictable routine. This will depend on the needs of your family. There’s no right answer.
Set up loving, appropriate boundaries. I don’t expect a toddler to stay seated at the table for 30 minutes, but I would expect a two year old to eat at the table for 10 minutes instead of taking a bite from the table and running around. If your child is on the autism spectrum, this may not be an appropriate expectation.
Harness the power of hunger. You’re more likely to have successful mealtimes if your kids come to the table hungry. Having a predictable schedule will help.
Make meal time social. Eating with your child, enjoying foods together and modeling appropriate mealtime behavior can help.
Limit the introduction to new foods. New foods are an important way to teach your child about healthy eating. Introduce something new together with something familiar to help your child acclimate.
How long does picky eating last?
Among children who are picky eaters, only about one-third to one-half will outgrow their picky eating within two to three years. Three to 10 percent of infants and children have significant, persistent feeding and/or growth problems over time. These are the children who have pediatric feeding disorder (PFD) and need feeding treatment.
When should I be worried about picky eating?
While picky eating is a common behavior among children, extreme picky eating can lead to nutrient deficiencies or poor growth.
Extreme picky eating is a sign of PFD if a child displays some of the following characteristics:
- Extreme food selectivity: based on texture, color and taste
- Food refusal: gagging, vomiting, hitting, crying
- Limited appetite
- Poor weight or failure to gain weight
- Delayed or dysfunctional eating skills
- Disruptive mealtime behavior
- Eats differently in different environments
- Negatively impacts family functioning
Children with PFD need medical intervention to manage the diagnosis. When a child isn’t eating or drinking the quantity or the variety they need to grow and be healthy, it’s not just because they are being “fussy.” There is usually an underlying reason. Talk to your pediatrician about PFD and check out our family roadmap for support.
Cuyler Romeo is director of strategic initiatives at Feeding Matters and a clinician at Banner-University Medical Center’s NICU.
Premature births on the rise, leading to more pediatric feeding disorders
Published by Feeding Matters on Jan 24, 2023
Here’s what you need to know about the stats on premature births in the U.S., its causes and what we can do about it.
For most families of babies in the NICU, a premature birth comes as a total surprise. That’s because nearly 90 percent of babies in the U.S. are born at gestation, after 37 weeks. But an increasing number of newborns are born prematurely, according to the March of Dimes 2022 Report Card, released in November.
A rising rate of premature births results in an increasing number of babies with feeding issues. Those children who develop long-term feeding issues are at risk of having a pediatric feeding disorder, or PFD.
With a rate of 10.4-10.7 percent of babies born prior to 37 weeks in the U.S. in 2021, the March of Dimes gave an abysmal preterm birth grade of D+. It’s a rate that’s .4 percent higher than the previous year and the highest recorded rate since 2007.

Globally, the rate of preterm birth ranges from 5 to 18 percent of babies born, according to the W.H.O.
The number of weeks babies are born prior to full term and the newborn’s health will determine how long families spend waiting for their babies’ release from the NICU. In an average week in the U.S., nearly 70,000 babies are born. Over 7,000 of them are premature.
Depending on how premature a baby is and problems that may have occurred during their stay in the NICU, most of those babies eventually go on to reach all the milestones of their full-term peers. But this unexpected start is distressing for parents. The biggest challenge for most of the babies is feeding.
NICU staff spend most of their time supporting preterm babies’ nutrition needs, says Dr. Matt Abrams, a neonatologist with Arizona Neonatology at HonorHealth Scottsdale Shea Medical Center. “Feeding difficulty is one of the most common and challenging things we deal with in the NICU. Although people think of preterm babies as having breathing issues, most of the time in the NICU, we spend on nutrition and transitioning to oral feedings.”
The duration of a preemie’s feeding challenges is inversely related to their gestational age. The more pre-term the baby, the more likely they are to take longer to mature. Upon release from the NICU, Dr. Abrams says most of these babies will start to eat normally after a few weeks at home. But some of them will continue to struggle with feeding challenges.
The annual prevalence of PFD in the United States is between 1:23 and 1:37 children under the age of 5. This is higher than other more well-known childhood conditions such as autism (1:54) and cerebral palsy (1:323). Not all children diagnosed with PFD were once preemies, but many of them were.
Causes of preterm births in the U.S.
There are several variables that determine whether or not a baby is born prematurely. These include the following:
- The age and health of the mother
- Contraction of COVID-19 while pregnant
- Obesity and hypertension
- Multiple gestation
- Proximity to a hospital
- Race
- Poverty
- Access to prenatal care
- Smoking/drinking/drug use
Among other contributing factors such as access to prenatal care, Dr. Abrams sees fertility treatment as a key reason for more premature births. “Some places are not being judicious about how many embryos they’re implanting, which leads to higher rates of multiple gestations and therefore increases risk of premature birth,” says Dr. Abrams.
Whatever the cause, an early delivery is a challenge and a shock for parents. This was the case for Paula Benzing, a mom of three in Mesa, Arizona.
Paula visited her doctor for stomach pain, indigestion and heartburn. These symptoms are common in pregnancy, but Paula’s case was severe. Her doctor ordered blood work, and she was diagnosed with HELLP, hemolysis, elevated liver enzymes and low platelet count.
Paula had a cesarean section right away, at 28 weeks. Her son, Isaac, who’s now 13, was in the NICU for 3.5 months. Much of that time, and for months afterward, was spent on feeding therapy and bottle therapy.

Paula’s second child was born at term. With her third, 6-year-old Penny, Paula once again had to deliver at 28 weeks. Penny needed even more feeding support than Isaac. She came home from the NICU with a feeding tube, which was replaced by a g-tube at six months.
Paula’s day revolved around feeding Penny, all while chasing a two-year-old toddler. Every three hours she’d thicken formula to attempt to feed Penny orally – knowing she wasn’t likely to take it. She’d toss out that formula and instead mix a thinner version for the g-tube instead. “No matter how slow we did it, most of the time she’d throw up. I was a big ball of stress,” says Paula.
Dr. Abrams sees countless anxious parents in the NICU who stress over their babies’ feeding progress. “Eating is social, so it’s very distressing to families when kids can’t do that. At the same time, it’s not very tangible. When babies are on a ventilator or they have something more concrete, families cope much better than when their baby is totally healthy but having feeding issues. They must be patient to see how things evolve over time.”
The increase in preterm births in the U.S. means more and more families are having to be patient. But, not all families are affected equally.
Race and geography matter for maternal health
In the March of Dimes report card, some states scored worse than others. Nine states and one territory, including seven states in the Southeastern United States, received a grade of F. Only one state, Vermont, received a A- state-level preterm birth rate, with the lowest preterm birth rate at 8 percent.
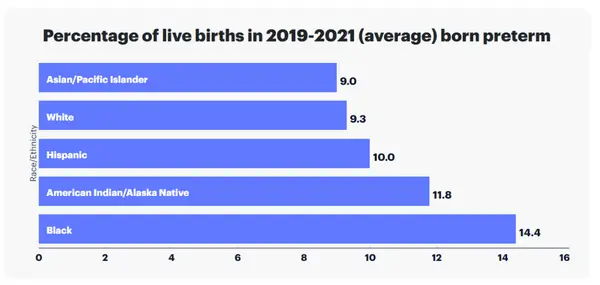
Preterm birth rate also varied by race and ethnicity in the United States. Preterm birth rate among Black women is 52 percent higher than the rate among all other women, according to the report.
Within states, the likelihood of preterm birth varies as well, depending on location, economics and ethnicity.
Impact preterm birth has on children and families
A preterm birth is often stressful for parents during their baby’s stay in the NICU. Juggling work and home responsibilities compounds that anxiety. Preemies are typically sent home with overwhelming and time consuming care instructions that can include multiple care appointments.
Parents of children who require longer support or have additional diagnosis, like pediatric feeding disorder, carry an even heavier burden.
According to a nationwide survey of insured families conducted by Feeding Matters:
- 76% of respondents reported that PFD results in at least a moderate financial burden for their family
- 33% of respondents had to leave full-time employment
- 23% turned down a job offer/raise in pay/more hours per week
- 47% reported depression
Overall, the lifetime average income loss to a family is $125,645.
The stress for a family can be tremendous for the duration of a child’s feeding challenges. Denise Hoffman is a pediatric occupational therapist and clinical assistant professor at Indiana University South Bend. While she was uniquely positioned to support her child who was born prematurely and had feeding issues, she still faced massive challenges. She had the luxury of quitting her job and made breastfeeding her son, Trey, a full time job. She describes feeding him and practicing feeding therapy a 24/7 job. Still, she recalls that he’d only manage to eat an ounce in a feeding.
Besides the time commitment this requires, the stress takes its toll. “As a mother your instinct is to feed your kid, and when you can’t, you feel like a failure,” she says.
Denise was grateful that she could stay home with her son and his older brother. She also had help from family. Many Americans facing similar struggles aren’t as fortunate.
How the U.S. can decrease the rate of preterm births
Prenatal care helps prevent preterm births. But Dr. Matt Abrams argues intervention needs to take place even before pregnancy.
“I think the work must be done before pregnancy by reducing complications related to obesity, diabetes and hypertension and by having fertility treatment that is judicious about who is a good candidate and how many embryos are implanted. Once you’re pregnant, there are few ways to reduce preterm birth other than good prenatal care. In rural areas of the country, it means increasing access to telemedicine.”
The March of Dimes advocates for much-needed legislation and funding that can improve maternal and infant health outcomes. Click here to read about their campaign #BlanketforChange to advocate for health equity for moms and babies.
They say it takes a village to raise a child. Turns out, it takes the will of a whole country to support newborns and their families.
Feeding Matters is the first organization in the world uniting families, healthcare professionals, and the broader community to improve the system of care for children with pediatric feeding disorder through advocacy, education, support, and research.
Finding Peace Where You Are
Published by Amber Mieras, Family Advisory Council Chair on Dec 08, 2022
Dear Friends of Feeding Matters,

When Jax was born, we were aware of his Down Syndrome diagnosis and were prepared for the traits we expected: low muscle tone, some heart concerns, and more. What we did not expect was at 8 days old to be walking back into the hospital with our first failure to thrive diagnosis. After 4 months of numerous appointments, medications, and sleepless nights and tears, we were back there again with our second failure to thrive. This was when we got Jax’s NG tube and officially began our feeding journey. We started feeding therapies, tested out different formulas, and tried every suggestion given to us to help Jax eat. After an open-heart surgery at 10 months old we hoped for feeding improvement. After a g tube placement, we prayed for better eating. After years of therapies, a tongue tie procedure, countless “practice” meals and food play sessions at home, we were still making very little progress. This was when I found Feeding Matters.
Life was such a blur at that time I don’t even remember how I stumbled upon the website. But what I do remember was the day my mentor, Heidi reached out to me. For the first time in years, as soon as we started talking, I felt heard and understood. Not just about the medical concerns, but the emotional struggles. It was obvious that Heidi understood what our family was going through.
Over the next few months, I read articles about feeding struggles, attended our first Feeding Matters conference, and continued to have chats with Heidi. I can remember talking to Heidi one afternoon, and asking her how she does it. Her response, “You just have to find peace where you are sometimes”. This is not what I wanted to hear, but it was what I needed to hear. It has taken me years to truly understand this statement.
As I reflect on the last few years, I have come to understand that I need to strive to have 3 main goals each day when it comes to our family’s feeding experiences.
1. Peace – I seek peace each day where Jax is with his feeding journey and how I can support him. I cannot fix this problem away, but I can go into each meal with a heart of gratitude with whatever success we have, no matter how small. And each night, I have to lay down and not replay the hard moments. I must wake up each morning with a joy of starting a new day.
2. Perspective – I have come to realize that I have to make a choice on how I set myself up to support Jax. I have begged and prayed for so many years for Jax to eat. And yes, I would love for him to, but I have started seeking positive food experiences for him and our entire family instead. By shifting my perspective to better match where we are in this process, I am finding that I am having more moments of celebration, and not so many of fear and disappointment.

3. Purpose – I have met so many amazing families through therapies, Feeding Matters, and just in my daily life that I wouldn’t have had to chance to meet if it wasn’t for Jax and his feeding struggles. I have realized that while I can’t control his pediatric feeding disorder, I can determine what my purpose will be in this journey. I choose to use my challenges and lessons I have learned to support other families going through similar experiences. I have been able to do this by mentoring families with the Power of Two program with Feeding Matters. I also choose to be open and educate others about what PFD looks like in our family by sharing Jax’s struggles and successes.
PFD is hard, it has been long journey, and our family is finding ways to navigate it as best we can. I am so grateful to have had the opportunity to connect with Feeding Matters to help us in our journey and grateful to all of you who support this very important organization. In this season of many feeding pressures, I hope you all can find comfort with where you are in your journey.
Sincerely,

Amber Mieras
Family Advisory Council Chair, Feeding Matters
This is a guest blog while Jaclyn Pederson, CEO is out on maternity leave.
Meet the 2022 Virtual Community Event Honorary Chair
Published by Feeding Matters on Sep 21, 2022
Meet Elizabeth Goodman, mother to Elliot, and 2022 Virtual Community Event Honorary Chair. Learn more about the event and how to register here.
 Early in my pregnancy with Elliot, I found out I had severe IUGR (Intrauterine growth restriction). As a result, I was closely monitored and had to undergo an early scheduled c-section. It was determined that she needed to come out at exactly 37 weeks. She was born healthy but at a very low birth weight of 4.14 lbs, which was less than 1st percentile.
Early in my pregnancy with Elliot, I found out I had severe IUGR (Intrauterine growth restriction). As a result, I was closely monitored and had to undergo an early scheduled c-section. It was determined that she needed to come out at exactly 37 weeks. She was born healthy but at a very low birth weight of 4.14 lbs, which was less than 1st percentile.
During her first year, Elliot had no issues with feeding. She breastfed and then transitioned to solids like I had come to expect for her feeding journey. Right at year 1, she started refusing all solids. We didn’t understand why or what was going on. My mind initially went to Autism because she seemed to have gross motor skill and speech delays. Our pediatrician dismissed my concerns. He said some kids are just picky eaters. I did some research on my own and enrolled in a two-year evaluation at local organization for Autism and early childhood development. It was advised that Elliot had gross motor skill and speech delays and we were referred to the children’s hospital’s developmental pediatrician and outpatient rehab.
 The Developmental Pediatrician ruled out Autism and diagnosed Ellie with hypotonia and sensory processing disorder. Throughout all of this, I was desperate for help with feeding and didn’t know where to find it. Her diet during this time consisted of milk, yogurt, and limited purees. We started feeding therapy as part of her overall Occupational Therapy, but it didn’t seem to be helping. Elliot would only eat a handful of solids. I was worried about her nutrition. Every day I struggled with what to feed her and how to get energy into her growing body. Every day I felt like a failure.
The Developmental Pediatrician ruled out Autism and diagnosed Ellie with hypotonia and sensory processing disorder. Throughout all of this, I was desperate for help with feeding and didn’t know where to find it. Her diet during this time consisted of milk, yogurt, and limited purees. We started feeding therapy as part of her overall Occupational Therapy, but it didn’t seem to be helping. Elliot would only eat a handful of solids. I was worried about her nutrition. Every day I struggled with what to feed her and how to get energy into her growing body. Every day I felt like a failure.
She slowly started accepting a few solids. I was scared to give her non-accepted foods for fear that she would refuse to eat. I lived in fear of feeding time. I was desperate every single day to be able to give her the nutrition she needed. She was no longer on the growth chart.
It was very difficult for me, a healthcare attorney and lobbyist with resources, to navigate the confusing web of finding a diagnoses and treatment. This always reminds me that others are probably struggling even more to get access and figure out what is going wrong. We have to find ways to make treatment more accessible and available to marginalized and underserved populations.
After a lot of research and referrals, I finally started seeing a pediatric gastroenterologist at the local children’s hospital. She was the first doctor to listen to me, believe me, and help me find meaningful solutions to feeding. She prescribed a nutritional supplement and Elliot’s weight started increasing. She was back on the growth chart and for the first time I felt hope.
We were then connected to Feeding Matters. At Feeding Matters, I found solace to know that I wasn’t alone. It wasn’t just me, it wasn’t my fault, and there were resources available. Feeding Matters connected me with a pediatric nutritionist and a pediatric psychologist, who we still see today. I also got connected to a new feeding therapist.
 Elliot is now almost 8. She’s 30th percentile for weight and 70th percentile for height. We still participate in feeding therapy and have made so much progress. She now eats lots of fruits, grains, dairy options, and…BACON! She loves bacon and we go through several packages a week. Can you blame her? It remains the only meat product but adding a single meat product was an enormous hurdle as it was her biggest aversion. Sometimes she lets us add spinach into smoothies. Previously, she would stealthily sniff out a single morsel of veggie we attempted to incorporate into anything. And while her growth continues to be supported by some nutritional supplements, I can now see a future where we won’t need it for long. For me, this is huge.
Elliot is now almost 8. She’s 30th percentile for weight and 70th percentile for height. We still participate in feeding therapy and have made so much progress. She now eats lots of fruits, grains, dairy options, and…BACON! She loves bacon and we go through several packages a week. Can you blame her? It remains the only meat product but adding a single meat product was an enormous hurdle as it was her biggest aversion. Sometimes she lets us add spinach into smoothies. Previously, she would stealthily sniff out a single morsel of veggie we attempted to incorporate into anything. And while her growth continues to be supported by some nutritional supplements, I can now see a future where we won’t need it for long. For me, this is huge.
With the help of Feeding Matters and the incredible providers who listened, believed, provided a safe space, and helped us find solutions, we have made incredible progress and are incredibly grateful. I am honored to chair the 10th Annual Community Virtual Event to help raise awareness, funds, and hope for families with pediatric feeding disorder.
Celebrating Wins – The Neiderer Family
Published by Feeding Matters on Dec 22, 2021
Join us as we celebrate wins, big and small, for families facing PFD! Today, we celebrate the wins of Danny Neiderer! Danny’s mom Robyn was on the first Family Advisory Council and has served as a contract coordinator for the Power of Two program.

Our son, Danny, was born with Silent GERD which turned into Failure-to-Thrive around his first birthday. He struggled with pain any time he swallowed food and meal aversions quickly became our family’s challenge daily. With the support of our feeding therapist and team of specialists, Danny eventually embraced feeding methods helping him to achieve daily nutrition.
Our first win was around his 3rd birthday when he began eating all of his meals without us struggling and counting each bite. Our second win was around the same time period when he finally made his weight back onto the growth chart around the second percentile! Danny had been in “negative digits” off the curve and not even placing on the growth chart since around his first birthday. This win for our family was HUGE! As a parent, I finally didn’t feel like a “failure” anymore! Our third win was around his 4th birthday when we successfully weaned him off of all nutritional supplements and medications. Danny was discharged from all regular specialist appointments and we finally began to believe that we had gotten control over this extremely challenging time in our life!
I can happily report that today, Danny is a healthy and thriving 13-year-old young man who is excelling in middle school, loves to indoor rock climb and swim, and enjoys spending time with his siblings and friends. Our family always tried to celebrate these “small wins” along the course of his journey!
Our family’s 4th win was finding Feeding Matters! Even though we didn’t connect with this incredible organization until the end of our most challenging years, it has been such a blessing to support other families going through similar life experiences.
Our life lesson in all of this: Live life one day at a time and always look toward the light at the end of tunnel! You are not alone!
Thank you for letting us celebrate with you, Neiderer Family!