Author: Feeding Matters
CONGENITAL HEART DISEASE + PEDIATRIC FEEDING DISORDER
Published by Renee Bergeron on Feb 15, 2018
For February, a time known for American Heart Month, National Wear Red day, and Valentine’s Day, Feeding Matters welcomes guest contributor Renee Bergeron, author of Little Earthling Blog. A mom of 14, Renee always dreamed of a peaceful home full of little feet, days spent on a lovely piece of property with a lush organic garden to supply our family’s needs. Instead, she “ended up with real, live children who often interrupt me, a black thumb and hunk of property that no one has time to keep up with.”

When our son, Apollo, was diagnosed with a heart defect at 18 months old we weren’t shocked we were relieved. Apollo had been suffering from mysterious symptoms that puzzled the doctors. He had failure to thrive, loud, raspy breathing and poor sleep. He had already had his adenoids removed which had not improved his sleeping, eating, or breathing as the doctors had predicted.
After a severe choking incident a MRI was ordered. That day we were told our son had a double aortic arch, a type of vascular ring. We were immediately plunged into the world of congenital heart defects. We were told he would need just a single, non-invasive surgery to repair the ring. We were told to expect a full recovering, immediate improvement in his eating and gradual improvement with his breathing.
But it didn’t happen that way.
Apollo’s first meal after his surgery was a success! He downed waffle pieces, a bit of egg, and some canned peaches. But by the time we were home two days later, his feeding issues were back. Apollo wanted to nurse constantly. Even though he was now 22 months old, he barely ate solid foods. Getting two or three bites in was a “good” meal. He grabbed at the food he saw on the table, would take a bite, and cry. I ended up spending most of my day nursing and trying to get bits of food into him.
Apollo had struggled to eat from birth. Initially we thought he was sleepy from his c-section birth. Then, at two weeks old, he had his tongue tie clipped. He still struggled. We took him to the doctor again and again. At ten months old we took him to a children’s hospital where we were told he had severe reflux and was allergic to milk. We stopped all milk products, added in meds for reflux, and he still lost weight. He was tested for celiac and cystic fibrosis. Both came back negative, so we continued to struggle. At 10 months old Apollo was hospitalized with RSV and pneumonia. But none of that explained his eating issues. By his first birthday he was skinny, fussy, and still dropping off the growth curve.
That is why, when he was diagnosed with congenital heart defect (and a “simple” one at that) we were relieved. But our story didn’t end after his “non-invasive” surgery. Six weeks after his surgery to divide the ring, he was in the hospital again where, over a five day period, a slew of tests were run on our curly-haired toddler. An Upper GI finally revealed an answer to his feeding struggles. The vascular ring had left a diverticulum (pocket of blood) that was compressing his esophagus. That same day we made the decision to have a feeding tube placed and a week later the surgery was done.
We never gave up on our son being able to be tube-free. Our immediate concern was to help him gain weight and get “full” after a feeding for the first time in his life. Adjusting to life with a tube-fed toddler wasn’t easy but we did it. I made it my personal goal to never have a day pass without him eating something orally.
We were told Apollo might have a feeding tube for the rest of his life. So we adjusted our expectations. We bought a large, sturdy stroller to take him hiking and camping. We tube-fed him where ever we happened to be. We were determined that he would not miss out on life.
Eventually, it took two more surgeries, a year of feeding therapy, patience and prayers, but at age six-and-a-half, and midway through first grade, our son had his feeding tube removed.
Today Apollo is a healthy seven-year-old who loves LEGO, books, pizza, chips, and ice cream.
* * *
If you have a child with pediatric feeding disorder, feeling overwhelmed is not unusual. Feeding Matters is committed to providing parents with the support and resources they need to deliver the best care to their children, including our parent-to-parent coaching program and on-demand knowledge center.
For more information about CHD, please visit the American Heart Association’s page on congenital heart disease.
Volunteer Spotlight: Hayley Estrem
Published by Feeding Matters on Apr 10, 2019
 It is with a deep appreciation for the time, commitment, and passion of our dedicated advocates and volunteers that Feeding Matters is launching a monthly Q & A series. They help with events, participate on committees, and coach in our Power of Two program. The advocate and volunteer spotlights will share the stories of our growing network of change agents, the driving force behind our vision to create a world where children with pediatric feeding disorders will thrive.
It is with a deep appreciation for the time, commitment, and passion of our dedicated advocates and volunteers that Feeding Matters is launching a monthly Q & A series. They help with events, participate on committees, and coach in our Power of Two program. The advocate and volunteer spotlights will share the stories of our growing network of change agents, the driving force behind our vision to create a world where children with pediatric feeding disorders will thrive.
As a registered nurse, Hayley’s primary research interests began with a desire to improve family-centered care for children with feeding problems and developmental disabilities. Since 2009, Hayley has been a member of UNC’s Feeding Flock, an interdisciplinary research team with a mission to partner with families to nurture young children with feeding difficulties. Hayley volunteers her time with Feeding Matters serving on committees dedicated to creating the educational program for our International Pediatric Feeding Disorder Conference and Poster Session.
Tell us a little bit about yourself!I am originally from Troy, Missouri and grew up on a lovely farm with my grandparents as neighbors. I got my bachelor’s degree in Nursing in 2002 and was an RN in acute care adult settings for about eight years. Now, I have a PhD in Nursing so I get to do a combination of teaching and research that I find very satisfying. I have three boys, 12, 9, and 6 years old. We moved to the east coast in Wilmington, NC, just about 2 months before hurricane Florence. We were very fortunate that all was well with our home, and while repairs and recovery will be ongoing, it is a beautiful and resilient community! We are glad to be part of it.
How long have you been a volunteer with Feeding Matters?Since 2011.
In which volunteer activities have you participated?I was a parent volunteer member of the Treatment and Research committee in 2011. Later, after I had finished my doctorate and had experience in research, I was happy to be part of the planning committee for the first poster session at the 2017 conference, and was a member of the poster session committee for the 2019 conference as well as serving on the 2019 conference planning committee. Recently I joined the PFD Alliance as the Research Pillar Chair.
What motivated you to become involved with Feeding Matters?I changed my career path when my son was born with serious feeding difficulty and a rare chromosome disorder. It was all pretty hard. There just weren’t resources that we needed to guide us. We struggled for a long time, and eventually found some of what we needed for my son when he was 2 years old (in 2008). Soon after that, I learned about Feeding Matters, and I also started my PhD program to do research with feeding and family care that would help other children and families to not have to experience the struggle. I got involved with Feeding Matters because I felt I shared the mission, and I appreciated that they were an organization started by parents. It is about the lived experience of caring for these infants and children day-to-day, as part of a family that has some other things to accomplish too. So, let’s aim for success in the family setting, with success defined by family members in partnership with healthcare providers!
What has been your favorite part of volunteering with Feeding Matters?Interdisciplinary work and resources that are gathered. Seeing how Feeding Matters can help families.
What sets Feeding Matters apart from other organizations?It brings professionals from all the disciplines involved with feeding care together in a place where parents and families have a strong voice.
TOGETHER WE CAN DO SO MUCH
Published by Debbie Simons on Feb 27, 2018
“Alone we can do so little; together we can do so much.” –Helen Keller
Growth is something that most nonprofits strive for, regardless of their size. Small nonprofits want to get big, big nonprofits want to get bigger. Let’s face it, every organization has to grow (at least a little bit) every year in order to accommodate the increased expenses that develop over time. But good organizations do not only grow to meet and exceed the needs of their clients, they take it one step further – creating system changes that directly affect the lives of those they serve.
As many non-profits who are fortunate enough to experience some success soon discover, just because you have arrived doesn’t mean you can rest on your laurels! Growing doesn’t mean just grappling with the same challenges on a larger scale. It means understanding, adjusting to, and managing a whole new set of challenges as well as new opportunities.
Organizational growth requires a lot of strategic planning and effort. During my career I have been fortunate to spend time in both corporate America and the not-for-profit world, which helped prepare me for my role of chief development officer at Feeding Matters.
Since taking on this new role, I’ve had the pleasure to get to know this vibrant, energized group of people who are contributing, at the highest levels, to this thriving organization. And while I am blessed to have three healthy children, I am reminded every day of how many celebrations and life’s pleasures revolve around food and how much I take for granted being able to easily share a meal with my family each and every night.
As all great organizations before us would attest, there is a time when all the stars start align and goals that felt like dreams start to become reality. For Feeding Matters that time is now. For the first time we are within reach of seeing Pediatric Feeding Disorder get its own standalone diagnose. Once that dream becomes a reality it will unlock doors to do much more: needed research, collaboration, insurance reimbursements for families, an education path for healthcare professionals, and system changes for families with children who suffer to eat every day.
Like any other great and lofty goal, it takes time, resources, and funding to cross the finish line. This year Feeding Matters will embark on a three-year, $3 million dollar campaign to ensure our goals do in fact become a reality.
It only takes a moment to make a true human connection, a connection that can generate good will, energy, and positive bonds. Each day we are given dozens of opportunities to give our time, our talent or our treasure to those in need. This year, more than ever, we are asking our community to get behind our mission and help us further advances in pediatric feeding disorder by accelerating identification, igniting research, and promoting collaborative care for the millions of children and families living with pediatric feeding disorder.
To help support Feeding Matters, please contact Debbie Simons at dsimons@feedingmatters.org.

National Nutrition Month
Published by Feeding Matters on Mar 05, 2018
Every year, the Academy of Nutrition and Dietetics supports a nutrition education and information campaign called National Nutrition Month®. National Nutrition Month® encourages research through credible, scientific-based food and nutrition information. In addition, it inspires people to make sound food choices, as well as informed physical activity habits.
One of four domains in the coordinated care model encouraging a collaborative approach to pediatric feeding disorder, nutrition is the foundation for growth and development. Whether your child eats by mouth or through a feeding tube, good nutrition allows children to thrive. It directly affects a child’s brain activity and capabilities, fine and gross motor skill development, and overall health and wellness. Poor growth and nutrition for children can lead to lifelong issues and difficulties.
This year, the theme for National Nutrition Month® is “Go Further with Food.” This could mean preparing meals at home, choosing a healthy breakfast or simply picking snacks that are more nutritious. Often, adopting a healthier life style also means less food loss and waste.
That can be difficult for families navigating pediatric feeding disorder. Kristi Meyer, author of the children’s book The Adventures of Team Super Tubie and Professor at Cornell College in Iowa, considers a 504 medical plan meeting with her son’s school an important step. “In addition to the practical questions about who can replace our son’s g-tube if it were to fall out while at school, there are the emotional and social concerns that we, as parents, have in wanting our son to be accepted by his peers, never excluded from activities, yet proud of his differences.”
“In spite of all these concerns,” adds Kristi, “we have also learned there is something very comforting and reassuring about the opportunity to meet face-to-face with his teachers and school nurse whom he will get to know so well and rely on to be his support and safe haven throughout his hours away from home.”
For more information on nutrition and pediatric feeding disorder, visit feedingmatters.org/growth-nutrition.
KEEPING AN EYE ON YOUR CHILD’S OVERALL DEVELOPMENT
Published by First Things First on Mar 12, 2018
 If you are a parent or caregiver of a child 5 years old and younger, you can make a difference by monitoring your child’s physical, mental, social, and emotional development and talking about what you see with your son or daughter’s health care provider. This is not a way to find something “wrong” with your child, instead, it should be viewed as a partnership opportunity between families and healthcare providers to keep your child developing in the best way possible.
If you are a parent or caregiver of a child 5 years old and younger, you can make a difference by monitoring your child’s physical, mental, social, and emotional development and talking about what you see with your son or daughter’s health care provider. This is not a way to find something “wrong” with your child, instead, it should be viewed as a partnership opportunity between families and healthcare providers to keep your child developing in the best way possible.
- Keep notes and document issues that you are concerned about.
- Take pictures of your child doing a specific task.
- Record audios or videos on your phone of behaviors that concern you.
- Write down your questions and take them with you so you remember what to ask and tell your child’s primary care provider during your appointment.
- Call the toll-free, statewide Birth to 5 Helpline (1-877-705-5437). Nurses and child development experts are available to talk with you about your child, give you tips on which milestones they should have achieved for their age, and help you decide if a follow up with your health provider is needed.
- Fill out the online Ages and Stages Questionnaire from Easterseals. This free screening tool includes a series of questions regarding your child’s development and behavior. Results are emailed to parents within a couple of weeks and are intended to be used to follow up with a health provider regarding any identified issues.
- Complete the online Infant and Child Feeding Questionnaire from Feeding Matters. This free tool helps you better understand your child’s feeding habits and identify any areas of concern. Results can then be shared and discussed with your child’s physician. Additional resources for family support can be found on the Feeding Matters website.
- Contact Raising Special Kids if you have a developmental concern you want addressed, or if you think your child needs screening or further assessment.
- Get in touch with Child Find at your local school district for assistance with screening or special education services.
* * *
Feeding Matters and First Things First are united in supporting the health and wellbeing of Arizona’s children by nourishing a family-centered, comprehensive, and collaborative early childhood system. To learn more visit firstthingsfirst.org.
EMOJIS, IPADS AND G-TUBES, OH MY!
Published by Jennifer Wilson on Mar 14, 2018
This article is reposted with permission from The ASHA Leader Blog.
Have you ever tried to imagine feeding and swallowing treatment from a young child’s perspective? You might remember early negative feeding experiences making treatment challenging. You also might not fully understand concepts like “appetite” or “hunger.” Most likely, you also don’t really get why you work on feeding or what short- and long-term goals mean.
Working with young children who don’t comprehend why you’re there and what you’re helping them achieve can add another layer of complications to an already delicate process. Especially when transitioning from a gastrointestinal tube (g-tube) to oral feeding.
Feeding treatment can feel like a curvy, unpredictable path without mile markers. As the Tin Man, Dorothy and the Scarecrow head down the yellow brick road in the “Wizard of Oz,” they anticipate meeting “lions, tigers and bears.” Much like this tale down a tumultuous road, overarching fear and anxiety can often create an obstacle in providing feeding interventions.
I find helping clients understand the big-picture goal motivates them to continue down the path of feeding treatment, even when it seems scary or uncomfortable. I often turn to technology to communicate with clients and families. Easily accessible technology like sending photos or the universal meaning of emojis allows me to communicate these goals with my young clients quickly and clearly.
For example, a normal daily eating routine for many families involves grazing. Parents feed kids and themselves when schedules allow with no evident meal times. Talking about what having an appetite means and feels like, what a meal looks like, and which foods are proteins, carbohydrates, fruits and vegetables can help lay the groundwork for helping families understand and achieve goals. Next, I help clients and their families move toward healthy eating patterns. Communicating those concepts with the help of photos and emojis makes understanding more immediate and can more actively engage families.
Here are some strategies I use to help children feel more comfortable with new foods, provide tangible mile markers, and help the journey from g-tube intake to oral feeding go more smoothly.
- Create a social story to help the child understand why they come to feeding treatment. The social story could begin with pictures of the medical events leading to g-tube placement, the process of increasing oral intake at home and in treatment, and information about getting their tube removed when they reach a specific level.
- Create weekly goals for different types of protein, fruit/vegetable and carbohydrate intake. Challenge your client to text or email food emojis once they take tastes or have experiences with these foods.
- Help clients identify how their body feels before and after food experiences and when gastric discomfort should concern them. Work on increasing their ability to communicate discomfort and considering alternatives to spitting out or moving away from food using photos of smelling, licking or playing with food. Or how about an emoji sticking out its tongue? Providing visual supports can also help you create a gastric discomfort scale by assigning the numbers one through five to various images of people with stomach aches.
- Educate clients in ways they can “reset” when they feel overwhelmed. Help them identify calming strategies when their sensory system becomes overwhelmed. Offer them images of scenes they like, such as beaches, mountains, animals or other calming imagery. Send a short video of yourself taking deep breaths that they can mimic, or perhaps find a video or song they like so they can sing along or just listen.
- Give clients immediate and frequent feedback by recording sessions and playing moments of success. Continue to communicate the purpose and long-term goals of treatment during each session.
As our feeding/swallowing clients and caregivers become engaged team members, treatment can be an adventurous trip. Unlike lions, tigers and bears, emojis and iPads can provide comforting connectivity when managing the transition from g-tube to safe, oral feeding.
 Jennifer Wilson, MA, CCC-SLP, is a clinical instructor at the University of Tennessee Health Science Center. She has more than 20 years’ experience serving clients with pediatric dysphagia in a variety of settings. She is also a Feeding Matters Community Ambassador and an affiliate of the ASHA Special Interest Group 13, Swallowing and Swallowing Disorders.
Jennifer Wilson, MA, CCC-SLP, is a clinical instructor at the University of Tennessee Health Science Center. She has more than 20 years’ experience serving clients with pediatric dysphagia in a variety of settings. She is also a Feeding Matters Community Ambassador and an affiliate of the ASHA Special Interest Group 13, Swallowing and Swallowing Disorders.
THE POWER OF TWO
Published by Feeding Matters on Mar 21, 2018
Parents of infants and children with pediatric feeding disorder may feel isolated and overwhelmed with the medical, emotional, financial, educational and social issues they face as they raise their child. In today’s video blog, Pinali Agrawal tells her experience with the Power of Two program. “It literally opened up a whole different world to me. I had been searching for such a long time, since my son was born, to try to find a group,” Pinali describes. “I was so thankful to find Feeding Matters and the Power of Two.”
FEEDING MATTERS NAMED BIZ BASH BENEFICIARY
Published by Feeding Matters on Mar 23, 2018
Have you heard? Biz Bash, CoBiz Financial’s signature event, has selected Feeding Matters as a 2018-2019 beneficiary!
Known for putting the FUN into FUNdraising, Biz Bash combines music, mingling, a unique silent auction, and delicious food all to raise money for a great cause. By selecting Feeding Matters, Biz Bash will provide immediate and long-term positive impact for children and families suffering from the devastating physical, emotional, and financial effects of pediatric feeding disorder.

For 11 years, Biz Bash has brought the who’s who of American music history to Arizona, including The Gin Blossoms, America, Lou Gramm, Starship, Eddie Money, WAR and the Pointer Sisters. In 2017, Biz Bash featuring Dennis De Young: The Music of Styx, generated $156,000 for its Arizona beneficiaries, A New Leaf and New Pathways for Youth.
Since launching in 2001, Biz Bash has distributed more than $5.5 million to Arizona and Colorado not-for-profits reaching children and families in underserved communities.
We look forward to sharing more as details are finalized for this year’s date and headlining entertainment… So stay tuned!
NATIONAL AUTISM AWARENESS MONTH
Published by Feeding Matters on Apr 02, 2018
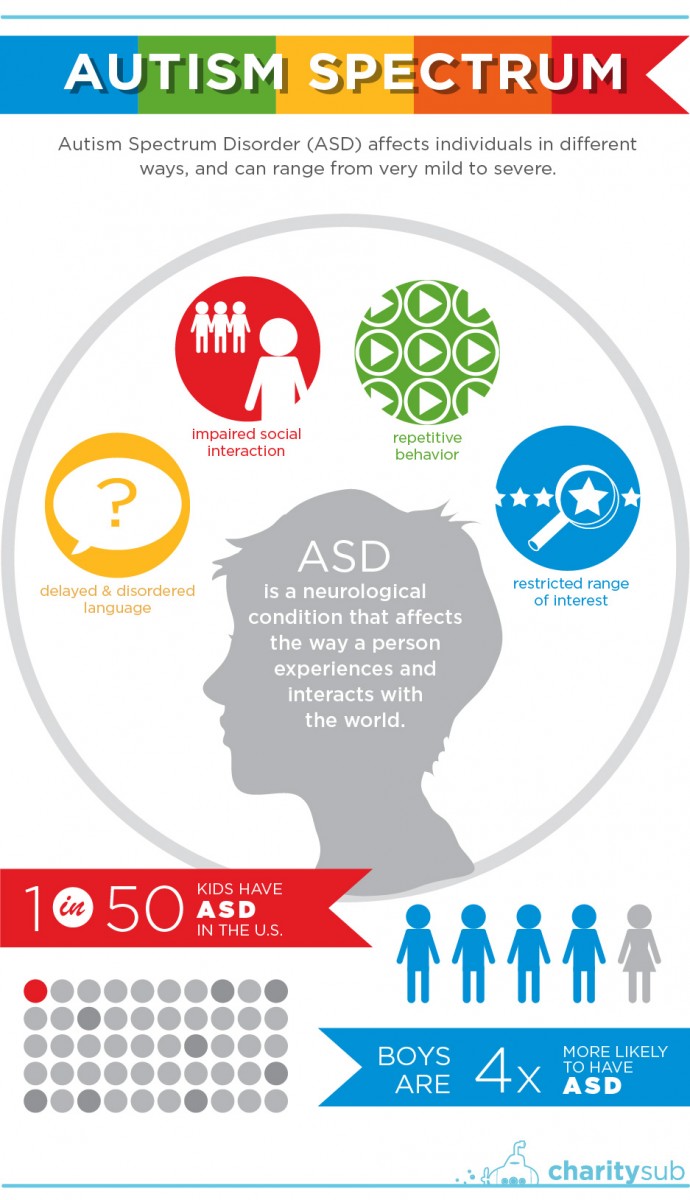
April is Autism Spectrum Disorder (ASD) Awareness Month. Started nearly a quarter century ago by the Autism Society, National Autism Awareness Month is “a nationwide effort to promote autism awareness, inclusion and self-determination for all, and assure that each person with ASD is provided the opportunity to achieve the highest possible quality of life.”
A neurological condition, ASD affects the way a person experiences and interacts with the world. With a national prevalence estimated at 1 in 50 children, ASD is one of more than 300 conditions that put children at a higher risk for pediatric feeding disorder.
STUDYING THE ECONOMIC BURDEN ON FAMILIES
Published by Feeding Matters on Apr 10, 2018
Over the years, Feeding Matters has witnessed many insured families spend hundreds, and sometimes thousands, of dollars out of pocket to cover non reimbursed costs related to their child’s pediatric feeding disorder. To fully and accurately capture the devastating financial burden related to pediatric feeding disorder, Feeding Matters began collecting data and testimonials from our families.
Determine the cost associated with out of pocket expenses for families. In order to further investigate the out of pocket expenses for families, Feeding Matters collaborated with FirstEval to create an Economic Impact Survey to collect data around the child and the family, including medical costs, supplies, lost income, child care, travel, education, time, parent/caregiver health, psychological impact, and demographic information related to pediatric feeding disorder. The results showed families are spending money on extra childcare, specialty foods, and travel to therapists to receive optimal care. This significant expenditure has drained many family’s bank accounts.
“We sold our home, moved to a rental house and ultimately had to file bankruptcy to be able to afford for me to work part time rather than full time and to afford my child’s weekly therapy visits. Even though I have a bachelors degree and professional career, I took a job as a nanny (making significantly less than I made previously) so that I could have the flexibility to take my child to therapy and to stay home with him when he was too sick to go to school. The pressure of trying to manage my full time job while he was sick and had so many appointments was simply too much for me.”Obtain data that will be used to help change the system of care and coverage around pediatric feeding disorder. The costs incurred by families navigating pediatric feeding disorder are not well understood by the reimbursement community and this has prevented them from being covered by most insurance companies. The data collected from the survey will be used to inform healthcare professionals and insurance companies of the financial burden of pediatric feeding disorder and influence the system changes that need to occur in order to obtain coverage for families. Feeding Matters is anxious to lead the way in helping families get the coverage they need.
It’s more than emotional stress that parents endure when their child has pediatric feeding disorder Money and finances continue to be top stressors for families managing pediatric feeding disorder. That stress, coupled with the emotional stress that families endure can be detrimental to one’s health. Families have indicated that they have heightened anxiety, difficulties in their relationship, and depression due to the financial stress of caring for a child with pediatric feeding disorder. When a parent is feeling these emotions, it is likely that their child will feel this too.
“I am killing myself trying to work full-time to support my daughter as a single parent. My parents had to move from out of state to help, and even with them here I am exhausted from trying to coordinate supplies, therapy, and her care while maintaining full-time employment. I want to quit and give up every day, but I can’t. It is maddening.”
Feeding Matters is currently looking at the findings and determining next steps for sharing this with the community.
Update: View more information here.