Author: Feeding Matters
Volunteer Spotlight: Jennifer Casteix
Published by Feeding Matters on Aug 06, 2019
Jennifer is an SLP living in Tucson, Arizona. Her help as a member of the conference committee and her efforts at our 2019 International Pediatric Feeding Disorder Conference were invaluable. She is passionate and fits perfectly with Feeding Matters.
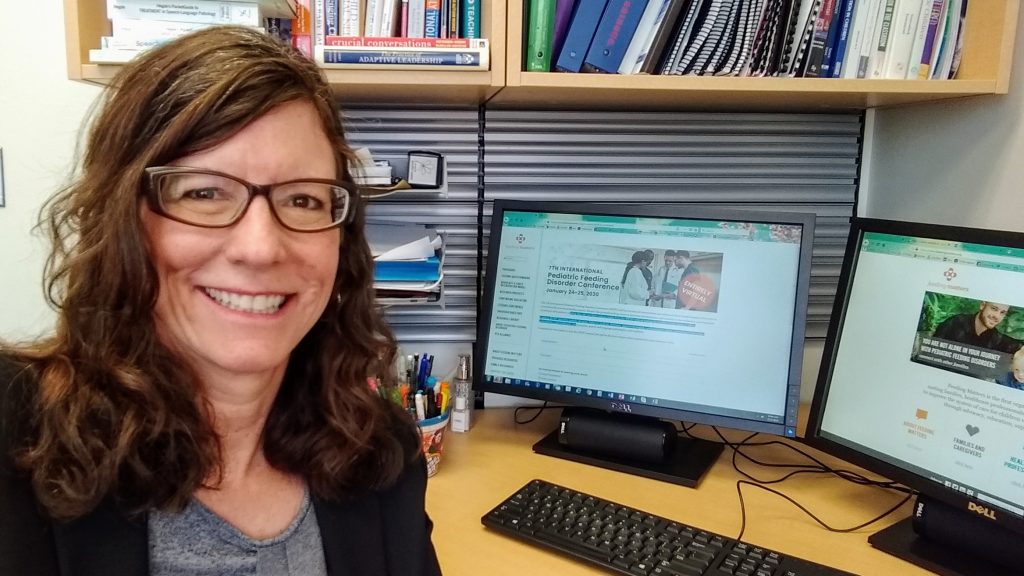
Tell us a little bit about yourself!
I received my master of science at The University of Arizona in 1989, and have worked with children with special health care needs (feeding and swallowing, neurodevelopmental disorders including autism) in Tucson and Southern Arizona ever since. I spent 20 years at Tucson Medical Center seeing infants and children in the NICU, PICU, and outpatient settings. I have been on the clinical faculty at the UA since 2009, where I also spent 5 years teaching graduate students and treating infants and children with dysphagia in the NICU and PICU at Diamond Children’s Medical Center. I teach graduate students in our on-campus clinic, and teach the graduate course in pediatric feeding and swallowing.
I’m married to George, who is the best traveling companion in the world. I am very involved in the volunteer community, including sitting on the boards of Community Food Bank of Southern Arizona, Komen Foundation Southern Arizona, Arizona Public Media, Tucson Festival of Books, and the Junior League of Tucson, Inc.
How long have you been a volunteer with Feeding Matters?
I have been a volunteer for 18 months, but I first met Chris and Shannon 10 years ago when they were first starting Feeding Matters (it was POPSICLE back then).
In which volunteer activities have you participated?
I sat on the program committee for the 6th International Pediatric Feeding Disorder Conference. I was the CEU administrator for SLPs attending the event.
What motivated you to become involved?
This is a cause that is near and dear to my heart. I have dedicated my career to working with children with feeding difficulties and their families, and training the next generation of practitioners. Feeding Matters supports this ideal.
What has been your favorite part of volunteering with Feeding Matters?
Meeting all of the wonderful people who work at Feeding Matters!
What sets Feeding Matters apart from other organizations?
I think it’s the people; all of the people involved.
Volunteer Spotlight: Gretchen Clavey
Published by Feeding Matters on Sep 04, 2019
Gretchen began volunteering as a family coach for Feeding Matters back in 2016. Raising 10 children and going back to school for nursing, she realized that she could help with awareness to the medical field by serving as a Feeding Matters Community Ambassador in her home state of Illinois.
 Tell us a little bit about yourself!
Tell us a little bit about yourself!I’m a wife and mom. Two years ago I decided to go back to school to become a nurse.
How long have you been a volunteer with Feeding Matters?
Involved since 2016, time has flown!
In which volunteer activities have you participated?
I started out with the Power of Two program because I really enjoyed working directly to support and encourage other families. After taking on more hours with school, I began serving as a Community Ambassador for Feeding Matters. As a Community Ambassador, I hope to help raise awareness about Feeding Matters and increase collaboration among families and health care professionals who serve children with pediatric feeding disorder.
What motivated you to become involved?
My youngest daughter has various medical issues including Down syndrome and a complex heart defect. She started out life completely tube fed and slowly gained the ability to eat solid foods by mouth. Over the past 6 years, she has taught me very important lessons in life about patience, acceptance, and celebrating small victories. I was looking for an opportunity to encourage others walking a similar path to myself and celebrate their child along with them.
What has been your favorite part of volunteering with Feeding Matters?
Working directly with other parents is the best part about volunteering. But I am also aware that we need more people involved as mentors and more health care providers who can collaborate in serving this population of children. As a Community Ambassador I appreciate the opportunity to help expand our outreach. I truly feel it is making a difference in the lives of children with PFD and want more of them to benefit.
What sets Feeding Matters apart from other organizations?
The twofold outreach to families as well as health care professionals is an excellent strategy to make an impact on the most children with pediatric feeding disorder. I also love the fact that Feeding Matters’ mission combines advocacy, support, education, and research. Progress in each of these areas is vital to improve the system of care that these children need and deserve.
Volunteer Spotlight: Dina Barnes
Published by Feeding Matters on Oct 25, 2019
Dina has been a volunteer with Feeding Matters since June of 2018. She is always willing to help, whether it’s at our annual community luncheon or with special projects, including coordinating all of the 2018 and 2019 Colten Cowell Foundation Cave Experiences and represents our organization at the events.
 Tell us a little bit about yourself!
Tell us a little bit about yourself!I live in Chandler with my husband, Tom, son Jackson, and playful dog Miley. Our daughter, Kendal, is currently a senior at ASU, living in Tempe and graduating in December. Jackson is a sophomore in high school. I was a teacher for 25 years, and just last year decided to take a break from full time teaching and get a “regular” job. ???? This choice has given me time to volunteer, work with kids one on one through tutoring, and spend more time with my family.
How long have you been a volunteer with Feeding Matters?
I have been volunteering for just about a year. I love it!
In which volunteer activities have you participated?
I help to coordinate the Colten Cowell Foundation Cave Experiences for Feeding Matters’ families, assisted at the 2018 luncheon, and have attended several community outreach events.
What motivated you to become involved?
I was invited to the 2017 luncheon by a friend, not really aware of what Feeding Matters was all about. After hearing the speakers I was absolutely awestruck…I knew I HAD to be involved in some way.
What has been your favorite part of volunteering with Feeding Matters?
There are so many amazing people working at Feeding Matters, I’m honored to have met them and have the opportunity to work with them.
What sets Feeding Matters’ apart from other organizations?
Feeding Matters fosters such an atmosphere of helping and caring…from the CEO all the way down to the volunteers. Everyone works so well together and are all working towards a common goal – to help families.
Volunteer Spotlight: Melissa Knight
Published by Feeding Matters on Nov 08, 2019
Melissa is one of our Power of Two family coaches in Ohio. She started volunteering back in 2014 as a regular contributor to our blog where she shared her journey with her daughters and brought so many families relief and hope.
 Tell us a little bit about yourself!
Tell us a little bit about yourself!I am married and a stay at home mom and homeschool teacher. I was blessed with two amazing girls. I enjoy spending time with my family, watching movies, reading, cooking, arts and crafts, exercising, and teaching.
How long have you been a volunteer with Feeding Matters?
I have been a volunteer with Feeding Matters since 2014.
In which volunteer activities have you participated?
I started volunteering by writing blogs for Feeding Matters. Once some of the feeding challenges settled down in our family, I wanted to do more and I became a Power of Two coach.
What motivated you to become involved?
I was motivated to become involved with Feeding Matters because my life revolved around trying to feed my children for many years. Both of my daughters had pediatric feeding disorder, starting in infancy and continuing for at least six years each. I saw firsthand how every single day was a struggle and how people outside of our family did not understand. From that moment forward, I knew I wanted to help other parents in similar situations. I also like to help families specifically, dealing with gastroparesis as well as cyclic vomiting syndrome since those issues are close to my heart.
What has been your favorite part of volunteering with Feeding Matters?
My favorite part of being a Power of Two coach is forming a bond with the family I am coaching. Some of the families have such similar stories like our family and we form this unspoken bond of understanding one another without even finishing sentences. We both know what it is like to live this struggle and I like to show that there is hope and a purpose to all of this. I try to be a beam of light in the darkness they are feeling.
What sets Feeding Matters apart from other organizations?
Feeding Matters is a wonderful organization. I think what sets them apart from other organizations is the passion they have for making a difference. From the very top, the lovely ladies that formed Feeding Matters were touched personally by pediatric feeding disorder and it shines through in the challenging jobs they have to bring awareness. Everyone I have ever worked with has enthusiasm and passion like I have never seen before. They love their jobs and therefore they make a difference. No matter what the pediatric feeding disorder involves, Feeding Matters has so many resources to help families find the support they need.
NICU Graduates: On Track for Ongoing Feeding Success!
Published by Allyson Goodwyn-Craine on May 28, 2019
As each little feeder prepares to transition from our 20-bed, level III neonatal intensive care unit (NICU) to home, the interprofessional team assigns them one of three tracks to support their feeding skills progression. We do this as part of the rounds our team participates in together each day.
This approach helps monitor feeding as babies mature, provides prompt intervention when needed, and supports our ongoing goal of reduced hospital readmissions associated with feeding.
Here’s how each track works to support our smallest patients:
Third track infants receive the guidance of our nurses and lactation nurses to advance their feeding skills. These babies are monitored through our general outpatient pediatrics services after discharge. The pediatrician, dietitian, and lactation registered nurse (RN) monitor the infant’s feeding progress. A neonatologist also calls to check in with the family shortly after discharge. If feeding concerns arise, any of these providers can initiate a referral for an outpatient feeding evaluation with a speech-language pathologist skilled in pediatric feeding and swallowing evaluation and treatment.
Second track infants require a feeding plan generated by our NICU SLPs, occupational and physical therapists (OT/PT) to support their feeding skills. Prior to discharge, they also recommend an outpatient referral to an SLP for continued feeding evaluation. The outpatient SLP works in collaboration with the pediatrician, lactation RNs, and pediatric dietitians as the infant continues to mature.
These infants benefit from specific and evolving interventions after discharge such as special positioning, pacing, or use of a special bottle/nipple they may soon outgrow. We might also make this type of referral for ongoing outpatient services to families who need added support to learn how to provide ongoing feeding intervention and support.
First (or fast) track infants require advanced clinical feeding evaluation by the NICU SLP. These evaluations can include videofluoroscopic or modified barium swallow studies. We also make a plan for treatment to address highly complex medical or feeding concerns often associated with swallowing, craniofacial, cardiac, ongoing endurance, and respiratory conditions.
Keeping the same NICU SLP—who follows the infant throughout their NICU course and develops first-hand knowledge of their feeding progress—creates seamless continuity of care during the transition to an outpatient with this same clinician. The SLP makes an initial outpatient feeding appointment for the infant “on the fast track” prior to discharge.
Some infants receive this follow-up care as soon as three days post-discharge, while others can wait up to two weeks depending upon their needs. The NICU SLP continues to follow the infant for feeding as an outpatient as clinically indicated.
Additional means of monitoring feeding progress
Pediatricians, pediatric dietitians, lactation nurses, and outpatient SLPs are on the front line in working with our NICU graduates.
All disciplines, including the outpatient SLPs, can provide phone, video, or in-office appointments based on the infant’s ongoing needs. Our hospital provides two types of NICU follow-up clinics: One has a neonatologist who monitors progress in collaboration with the infant’s pediatrician. Our multidisciplinary NICU follow-up clinic provides a neonatologist, physical and occupational therapists, pediatric dietitian, social worker and NICU/outpatient SLP. This team monitors overall development and continues to educate and support the family.
Our low-birth-weight infants automatically quality for early intervention services. Anyone on the team can also generate early-intervention referrals when sensory, motor, or other developmental concerns are observed at any time along the way.
Our outpatient pediatric feeding SLPs also receive feeding evaluation referrals from a variety of sources outside the NICU. We work closely with inpatient speech-language pathology colleagues at our local children’s hospitals when infants transfer to our care. In addition, area pediatricians, family practice physicians, lactation RNs, dietitians, head/neck surgeons, and motor therapists do a great job of monitoring feeding progression and weight trajectory in order to direct infants our way anytime they require additional clinical feeding support.
It truly is a collaborative team effort to keep our smallest patients on track for feeding success!
Allyson Goodwyn-Craine, M.S., CCC-SLP, BCS-S, works in the neonatal intensive care unit and outpatient rehabilitation services at Sunnyside Medical Center in Portland, Oregon. She is also an adjunct professor at Portland State University and a guest lecturer at Pacific University.

Register Now: 2019 Virtual Town Halls
Published by Feeding Matters on May 21, 2019
Can you say EOSINOPHILIC? (E-O-sin-O-fill-ik)
Published by Feeding Matters on May 17, 2019
 The body’s immune system serves as its own internal ambulance, responding to crisis and triaging needs as they arise. Most times that rapid response works out just fine.
But sometimes, the immune system can turn on the body, or become a little too overzealous with its treatment to a perceived emergency, which can lead to other problems. An eosinophilic disorder is one of those.
Eosinophil-associated diseases are not only hard to pronounce, they are often difficult to diagnose due to a lack of awareness about the chronic digestive conditions. And that’s one of the reasons why National Eosinophil Awareness Week, held every year during the third week of May, is important.
At Feeding Matters, we’re acutely aware of how eosinophilic disorders impact the lives of those living with them, from children to adults. And we understand how challenging it can be to navigate, treat, and manage a chronic condition that affects eating and feeding.
Eosinophils are naturally-occurring white blood cells that, when they’re doing their jobs correctly, respond to allergy-triggering foods or allergens and release toxins to combat a reaction. But sometimes the body makes too many eosinophils.
When they build up, beyond the normal 5-percent volume of a person’s white blood cells, they trigger inflammation. And that leads to tissue damage.
Eosinophilic disorders are most often diagnosed in the esophagus, the stomach, the small and large intestines, or throughout the blood. Most eosinophilic disorders are endocrine or allergy-related and can affect the gastrointestinal, respiratory, and genitourinary tracts.
As one would expect, symptoms associated with eosinophilic disorders range based on where the inflammation and tissue damage is occurring. But, a number of common symptoms include difficulty swallowing, food getting stuck in the esophagus while eating, persistent heartburn, abdominal pain, vomiting, diarrhea, and nausea.
In children, eosinophilic disorders often result in a parent who experiences difficulty feeding and a child who has a difficult time eating. It is also noted that children who live with an eosinophilic disorder demonstrate a noticeable failure to thrive.
Due to the type of symptoms that come with eosinophilic disorders, it isn’t uncommon for those living with it to miss work or school.
While eosinophilic disorders are considered rare, it is an emerging problem worldwide and healthcare professionals are growing increasingly more aware of how the symptoms present themselves. Depending on the type of eosinophilic disorder, a diagnosis can come by way of a blood test, an endoscopy, or a biopsy of tissue. According to the American Academy of Allergy, Asthma and Immunology, physicians treat those diagnosed with an eosinophilic disorder by using a food elimination diet, corticosteroid medication to treat inflammation, and proton pump inhibitors to treat acid production in the stomach.
To learn more about eosinophilic disorders, how they impact the lives of those living with them, and how to manage chronic conditions associated with them, the American Partnership for Eosinophilic Disorders is a great resource.
The body’s immune system serves as its own internal ambulance, responding to crisis and triaging needs as they arise. Most times that rapid response works out just fine.
But sometimes, the immune system can turn on the body, or become a little too overzealous with its treatment to a perceived emergency, which can lead to other problems. An eosinophilic disorder is one of those.
Eosinophil-associated diseases are not only hard to pronounce, they are often difficult to diagnose due to a lack of awareness about the chronic digestive conditions. And that’s one of the reasons why National Eosinophil Awareness Week, held every year during the third week of May, is important.
At Feeding Matters, we’re acutely aware of how eosinophilic disorders impact the lives of those living with them, from children to adults. And we understand how challenging it can be to navigate, treat, and manage a chronic condition that affects eating and feeding.
Eosinophils are naturally-occurring white blood cells that, when they’re doing their jobs correctly, respond to allergy-triggering foods or allergens and release toxins to combat a reaction. But sometimes the body makes too many eosinophils.
When they build up, beyond the normal 5-percent volume of a person’s white blood cells, they trigger inflammation. And that leads to tissue damage.
Eosinophilic disorders are most often diagnosed in the esophagus, the stomach, the small and large intestines, or throughout the blood. Most eosinophilic disorders are endocrine or allergy-related and can affect the gastrointestinal, respiratory, and genitourinary tracts.
As one would expect, symptoms associated with eosinophilic disorders range based on where the inflammation and tissue damage is occurring. But, a number of common symptoms include difficulty swallowing, food getting stuck in the esophagus while eating, persistent heartburn, abdominal pain, vomiting, diarrhea, and nausea.
In children, eosinophilic disorders often result in a parent who experiences difficulty feeding and a child who has a difficult time eating. It is also noted that children who live with an eosinophilic disorder demonstrate a noticeable failure to thrive.
Due to the type of symptoms that come with eosinophilic disorders, it isn’t uncommon for those living with it to miss work or school.
While eosinophilic disorders are considered rare, it is an emerging problem worldwide and healthcare professionals are growing increasingly more aware of how the symptoms present themselves. Depending on the type of eosinophilic disorder, a diagnosis can come by way of a blood test, an endoscopy, or a biopsy of tissue. According to the American Academy of Allergy, Asthma and Immunology, physicians treat those diagnosed with an eosinophilic disorder by using a food elimination diet, corticosteroid medication to treat inflammation, and proton pump inhibitors to treat acid production in the stomach.
To learn more about eosinophilic disorders, how they impact the lives of those living with them, and how to manage chronic conditions associated with them, the American Partnership for Eosinophilic Disorders is a great resource. FAACT(S) About Food Allergies
Published by Feeding Matters on Apr 26, 2019
Millions of people live with food allergies and the guessing game that comes with diagnosing them and avoiding the foods that trigger a reaction.
It’s a well-documented struggle for adults who are able to communicate their symptoms and track their reactions to certain foods. But, it can be an exponentially more difficult road when parents are relying on a child to try and verbalize reactions that can’t be seen, such as respiratory difficulties and gastrointestinal issues.
One of more than 300 conditions that put children at a higher risk for pediatric feeding disorder, food allergies can often be misconstrued as an intolerance to a certain food, general pickiness or other chronic conditions by those who don’t fully understand the gravity of the condition. That’s part of the reason why Feeding Matters so appreciates Food Allergy Awareness Week, recognized May 12-18. It allows for an opportunity to educate the public and it offers a space for conversations, tolerance and understanding.
An estimated 6 million children are living with food allergies in the U.S., according to the Food Allergy and Anaphylaxis Connection Team (FAACT). And, only eight foods are responsible for 90% of all food allergies, according to FAACT. Statistics reported by the Journal for the American Medical Association indicate that shellfish, milk and peanuts are the top-three most common culprits of food allergies, followed by tree nuts, fin fish, eggs, wheat, soy and sesame.
Someone who lives with a food allergy can suffer a number of reactions, ranging from a rash to severe respiratory distress. In fact, experts estimate that a food allergy sends someone to an emergency room once every three minutes. And, the situation seems to be escalating in recent years.
Anaphylactic reactions have increased nearly 400 percent over a 10-year period between 2007 and 2016, and about 40 percent of children living with food allergies experience a severe and sometimes anaphylactic reaction, according to Food Allergy Research and Education (FARE).
Those who are forced to navigate life with a food allergy are also required to maintain a pretty consistent state of vigilance. That’s one of the reasons that schools place restrictions on the types of treats that can enter a classroom, and why some airlines have stopped serving peanuts as mid-flight snacks.
Knowing that trace amounts of an ingredient or cross-contamination could trigger a reaction, most people living with food allergies are advised to avoid buffets and deli stations, bakeries, ethnic restaurants because of potential language barriers, and Asian cuisine due to its liberal use of peanut-based foods and oils.
It is, however, possible to eat out with a food allergy. As awareness of the condition improves, so too does general tolerance for it and those who live with it. Restaurants are increasingly providing allergy information on their menus, and relationships with servers and restaurant owners make those conversations easier to have.
For more information about food allergies, we encourage you to visit these resources:Food Allergy and Anaphylaxis Connection Team
Food Allergy Research and Education
Kids With Food Allergies

Advances in Practice: Implementing the IDDSI
Published by Feeding Matters on May 01, 2019
 From 2013 through 2014, the IDDSI engaged in international systematic review and solicitation of stakeholder input, which included health professions, patients and caregivers, industry and researchers. The results? In 2015, the IDDSI panel ultimately created standardized guidelines for describing and determining food and liquid consistency. The IDDSI classification has eight levels, 0 through 7. A simple timed measure of the gravity flow rate from a 10ml syringe is used to classify liquids. The IDDSI website provides free, open access instructions with training videos on how to classify liquids based on this testing method.
Families and professionals alike now have access to shared terminology and an easy cost-effective and reliable method of determining food and liquid consistency. Visit the IDDSI website for downloadable handouts, instructions, and videos on how to implement the internationally endorsed IDDSI. The Academy of Nutrition and Dietetics also offers an IDDSI Boot Camp, including a monthly step-by-step plan for implementing the IDDSI in your workplace or community.
From 2013 through 2014, the IDDSI engaged in international systematic review and solicitation of stakeholder input, which included health professions, patients and caregivers, industry and researchers. The results? In 2015, the IDDSI panel ultimately created standardized guidelines for describing and determining food and liquid consistency. The IDDSI classification has eight levels, 0 through 7. A simple timed measure of the gravity flow rate from a 10ml syringe is used to classify liquids. The IDDSI website provides free, open access instructions with training videos on how to classify liquids based on this testing method.
Families and professionals alike now have access to shared terminology and an easy cost-effective and reliable method of determining food and liquid consistency. Visit the IDDSI website for downloadable handouts, instructions, and videos on how to implement the internationally endorsed IDDSI. The Academy of Nutrition and Dietetics also offers an IDDSI Boot Camp, including a monthly step-by-step plan for implementing the IDDSI in your workplace or community. 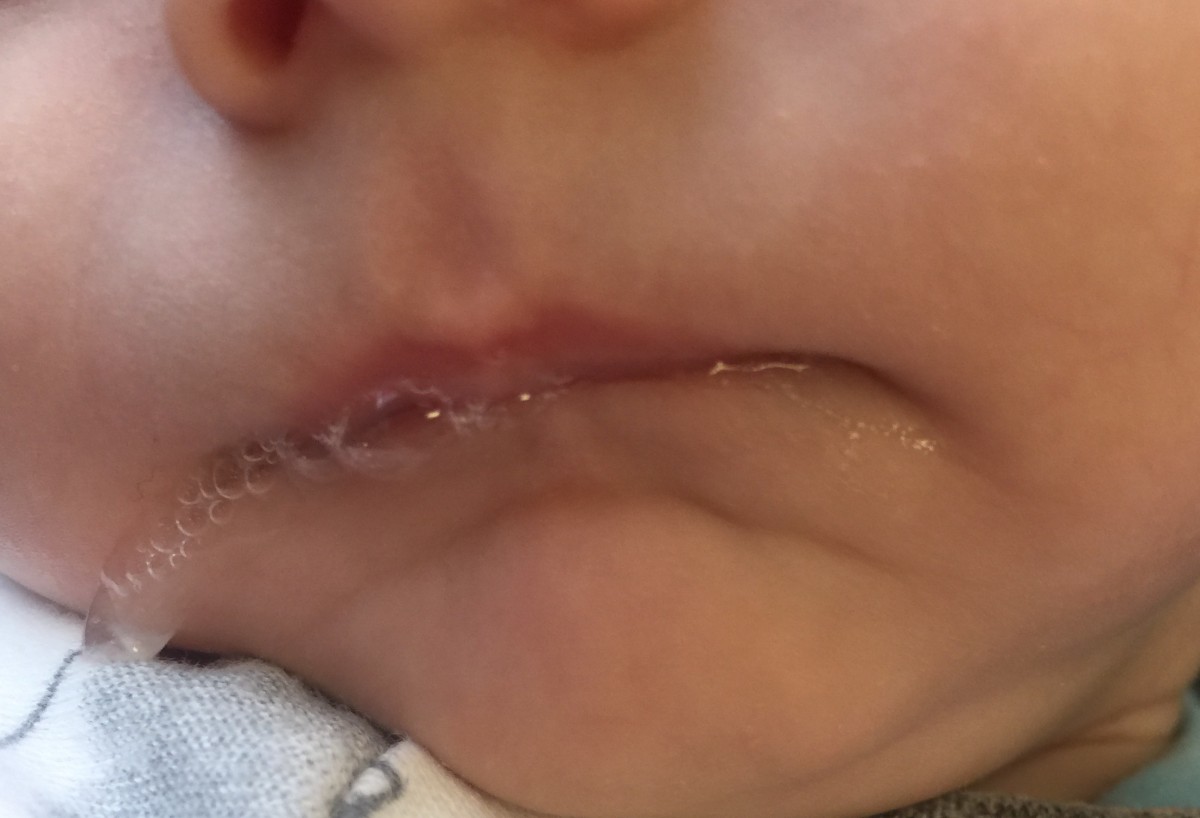
Feeding Infants with Recessed Jaw or Retrognathia at Breast or with Bottle
Published by Allyson Goodwyn-Craine on Jun 10, 2017
Infants with recessed jaw/ retrognathia present with unique feeding challenges and are sometimes misdiagnosed with ankyloglossia or tongue tie. This is of particular concern, because in some cases a frenulectomy is contraindicated. Although the anterior maxillary and mandible alignment is impacted, the primary concern is the tongue sitting posteriorly toward the pharynx. In severe cases airway obstruction can occur but milder cases also require consideration for airway patency. These babes often present with stridor reflective of increased respiratory effort but when paired with a confirmed diagnosis of laryngeal or tracheal malacia adequate respiratory support needed for sustained energy and coordination for feeding are frequently compromised.
The discrepancy between the maxilla and mandible often cause the nipple and areola to compress with anterior rotation. The position of the tongue can also inhibit elevation and retraction of the posterior tongue needed to recreate adequate inner oral pressure during the suck needed to efficiently draw milk from the breast. These oral mechanics can cause irritation to the nipple or tissue trauma or they have difficulty transitioning off of nipple shields sometimes mistaken as characteristic of ankyloglossia (tongue-tie). Many babes have improved latch in this position as gravity assists with tongue and occasionally jaw forward.
Detection of a recessed jaw can be a bit challenging. Infants naturally have a slightly recessed chin/jaw as part of normal development; however, those that present with a gap of 3 mm or more between the anterior upper and lower gum line often struggle at breast. These infants sometimes have prominent chins with a horizonal crease between the mental region and the lower lip. The lower lip often rests tucked behind the upper lip or superior alveolar ridge. Observation at breast and bottle will also reveal increased facial tension particularly along the lateral orbicularis oris often resulting in a narrow latch as the babe tries to compensate for anterior rotation of the nipple between the upper and lower gum lines. In more involved cases the infant struggles with the extension reflex of the tongue needed for latch stability as gravity pulls the back of the tongue posteriorially.
The good news is that positioning adjustments have proven very helpful, particularly at breast to use gravity to move the tongue anteriorly in the mouth creating additional pharyngeal space. For babies without sternal precautions or poor respiratory endurance I suggest a trial with Mom reclined with babe in prone position (also known as tummy to tummy, laid back or biological position). I find most success with placing a rolled bath towel or narrow end of the Gia or breast feeding pillow at babe’s chest allow them to come down onto the nipple without head extension. The breastfeeding pillow can also provide support through the baby’s hips as they rest in a tucked position in the center of the pillow with the lower inside edge supporting their bottom. It is not uncommon to hear less stridor in this position as a result.
For bottle feeding, elevated side lying with slight anterior rotation at the hips) or high cradle (with hips slightly forward, not directly under the shoulders) can work nicely. These positions also provide nice support for respiration. I personally prefer placing babe in classic football hold but rotate their hips and shoulders so they are “stacked” which also places the babe at a nice angle with space for the bottle and supports lots of yummy eye contact/engagement.
When bottle supplementation is needed, the Playtex Drop In Nurser with the Natural Latch nipple provides nice support along the jaw when the bottle is held at a slight angle to allow the lower edge of the nipple along the lower lip. I typically prefer this bottle/nipple for breast feeding infants to match the gape/latch that compliments oral positioning at the breast. Infants with small gaps between the maxilla and mandible typically show no concerns for breathing. However, infants with wide gaps require careful monitoring. If an infant demonstrates any stress responses in supine, parents report concern for potentially obstructive noises during sleep or the young infant spontaneously moves themselves from their back to side lying a sleep study and/or airway patency assessment should be done by an otolaryngologist (ENT). The infant’s pediatrician needs to be aware of these concerns for consideration of positioning for sleep.Some pediatricians may consider elevated or side lying sleep positioners specifically designed for these purposes. These should only be used under the direction of the physician.
The majority of infants with a slightly recessed jaw outgrow these feeding concerns. At around 3-4 months of age the infant’s neck elongates and the pharynx deepens as the jaw moves forward with facial growth. This brings the posterior tongue slightly forward with increased space allowing for functional tongue elevation and retraction. At this point most infants can transition to more traditional breastfeeding positions.
About Allyson Goodwyn-Craine
 Allyson Goodwyn-Craine (Ally) began her career in 1989. She is a Neuro-Developmental Treatment (NDT) trained Pediatric Speech-Language Pathologist/Feeding Specialist who has worked in Private Practice, Shriner’s Children’s Hospital, Randall Children’s Hospital, and now at Kaiser Sunnyside Medical Center. Ally enjoys helping medically complex babies and toddlers who struggle with feeding challenges from breast, bottle, and tube feedings to transitioning to solid foods. Ally joins infants, toddlers, and their parents in the NICU, NICU Follow-Up Clinic, outpatient treatment, and as a member of the Cleft Palate team.
Allyson Goodwyn-Craine (Ally) began her career in 1989. She is a Neuro-Developmental Treatment (NDT) trained Pediatric Speech-Language Pathologist/Feeding Specialist who has worked in Private Practice, Shriner’s Children’s Hospital, Randall Children’s Hospital, and now at Kaiser Sunnyside Medical Center. Ally enjoys helping medically complex babies and toddlers who struggle with feeding challenges from breast, bottle, and tube feedings to transitioning to solid foods. Ally joins infants, toddlers, and their parents in the NICU, NICU Follow-Up Clinic, outpatient treatment, and as a member of the Cleft Palate team.
Allyson served on the Financial Planning Board of the American Speech-Language-Hearing Association. She is a past president of the Oregon Speech-Language-Hearing Association. She has served on the advisory board and as an adjunct professor at Portland State University for 19 years and is a guest lecturer in Pacific University and University of Oregon graduate programs. She has also traveled nationally and taught as a member of the Education Resources clinical faculty. Allyson was recently awarded the Honors of the Association by the Oregon Speech-Language-Hearing Association.
Click here to contact Allyson