A story of triumph over pediatric feeding disorder
Published by Feeding Matters on Feb 15, 2024
The way pediatric feeding disorder (PFD) manifests in each child is as varied as the children themselves. But so many stories of parenting children with PFD are the same.
An infant struggles to feed and gain weight. Parents work tirelessly to feed their children and juggle medical visits. They search in the dark for a diagnosis of a complex problem they don’t understand, all while feeling alone and at fault.
Raising a child with PFD is a journey that rarely has a final destination. With the right support and care, it does get easier. This is the story of one mom of a son with PFD and how she’s gone from seeking help to supporting others.
One family’s journey with PFD
From the start, Erin Avilez’s son, Julian, struggled to breastfeed and gain weight. Her doctors were concerned about her baby’s measurements throughout her pregnancy. When her amniotic sac fluid was low, Avilez was induced at 37 weeks.
Julian was born at 5 pounds and right away had trouble sucking and taking in enough food at each feeding. Avilez switched to bottles, but Julian continued to undereat. “Within the first few months, there were already red flags that he was underweight and not getting enough nutrition,” she says.
Avilez and her husband started by switching formulas to see if Julian had some sensitivity to some ingredients. Still, they didn’t see much weight increase. Things got worse when her pediatrician sent Julian to a pediatric gastroenterologist. “That’s kind of where the horror of the story started,” she says.
Julian’s pediatrician and the GI weren’t communicating or working together and sometimes had different goals. “The GI’s only goal was for Julian to gain weight and cared less about how it affected his feeding,” says Avilez.
Julian got a nasogastric tube (NG tube) at three months old. The increase in calories made him vomit a lot, and he regularly pulled the tube out. Any time he pulled the tube out, Avilez would have to call her husband to come home from work so the two of them could force the tube back in. Insurance only covered a few tubes, making this devastating ritual even more difficult. Julian developed an oral aversion that he never had before and wouldn’t even let his parents touch his face. By seven months, Avilez insisted the NG tube be removed.
When Julian’s GI recommended a gastrostomy feeding tube (G-tube) instead, Avilez knew they needed a second opinion. Julian took some formula and solid foods orally, and Avilez thought they could build on that. A new GI at Phoenix Children’s Hospital agreed.
With a new pediatrician and GI, Julian’s doctors started working on finding a diagnosis. He was also able to join their intensive feeding therapy program. “The new GI doctor we saw listened, and he offered empathy and support,” says Avilez.
When Julian was 3.5, his family finally got a diagnosis of what caused his pediatric feeding disorder. A liquid and a food study showed that he has gastroparesis, a condition where the stomach muscles do not work properly to empty waste.
Now that Julian has a diagnosis, he’s able to take medication to help his gastric delayed emptying, as well as an appetite stimulant. He also drinks Ensure Clear to add more calories to his diet. Julian has an aversion to any formula or dairy because of his early experience with the NG tube.
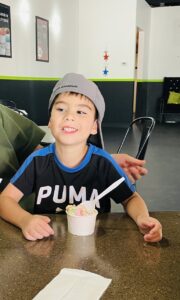
In the past six months, Julian was finally registered low on the weight chart for the first time. “This is huge for him,” says Avilez.
Still, says Avilez, their struggle is never far from her mind. She dreads visits to the pediatrician when she knows Julian will be weighed. “Even today, a week before his appointments, I start getting stressed out because I know we have to get on the scale,” she says.
Finding support from other families with PFD
Julian was born during the pandemic, and Avilez left her job as a social worker to take care of him and to get to all his appointments. She suffered from postpartum depression and felt overwhelmed, alone and isolated.
“I knew there has to be some type of service out there to help moms like me,” she says.

Avilez searched online and found Feeding Matters. She requested a peer-to-peer mentor and was matched with another mom who shared her experience. That empathy was powerful. “She listened to me. The first time I got off the phone with her, I started crying that somebody understood what I was going through,” says Avilez.
Avilez’s mentor also told her she was doing a great job. “Throughout this process, nobody told me I was doing a good job, not the doctors or anyone on his care team,” she says.
Avilez’s introduction to Feeding Matters was the first time she learned about PFD. “I felt so validated that we weren’t the only ones concerned about not knowing what was going on with our son and not hearing about it from our doctor,” she says.
Today, Avilez is a peer mentor to other parents raising a child with PFD. She’s grateful to have support and to be able to pay it forward. Her hope is that more clinicians and hospitals will inform parents about PFD from the start. “I wish that when you have a child with feeding difficulties, someone from the start would offer resources,” she says.
Key takeaways for supporting your child with PFD
Avilez offers the following advice to parents raising a child with PFD.
- Find a supportive care team: If the doctor’s not listening, find a more supportive provider. Having a good team in place makes all the difference.
- Trust your instincts: It’s okay to get a second opinion and ask questions. Keep advocating for your child because you know your child best.
- Find friends, family or a peer mentor: Find someone who will listen and understand so that you feel less alone.