Author: Feeding Matters
Join Us October 3 for Arizona Biz Bash 2019
Published by Feeding Matters on Aug 28, 2019
 2019 marks a new chapter for the iconic Biz Bash as part of the BOK Financial family. For the past 12 years, this good time for a great cause has made an indelible difference in our community and become one of the most recognized events in the metro area.
With a new brand in tow, the BOK Financial Biz Bash is still the official black T-shirt event, offering less programming and more fun, all while raising much-needed dollars for children and families in need in our local communities.
Since its inception, Biz Bash has distributed almost $6 million to local nonprofits in Arizona and Colorado, impacting thousands of children and families. It’s the perfect event for client entertainment, employee appreciation or networking.
2019 marks a new chapter for the iconic Biz Bash as part of the BOK Financial family. For the past 12 years, this good time for a great cause has made an indelible difference in our community and become one of the most recognized events in the metro area.
With a new brand in tow, the BOK Financial Biz Bash is still the official black T-shirt event, offering less programming and more fun, all while raising much-needed dollars for children and families in need in our local communities.
Since its inception, Biz Bash has distributed almost $6 million to local nonprofits in Arizona and Colorado, impacting thousands of children and families. It’s the perfect event for client entertainment, employee appreciation or networking. 
Introducing LACI: Learning Advanced through Collaborative Initiatives
Published by Feeding Matters on Sep 06, 2019
- Therapists will be able to utilize a local network for collaboration and expertise/advice.
- Referrals to the proper healthcare provider will be made more accurately and effectively, thereby decreasing waitlists for medically fragile children.
- Enhanced collaboration through a highly skilled cohort of medical professionals will enable enhanced care.
- Licensed OTR or SLP in good standing
- Currently or previously employed in a pediatric setting
- Strong commitment to professional growth and community partnering
- Statement of commitment: minimum of 4 hours per month to be allocated to collaborative goals
- Attend an in-person LACI launch meeting on October 22, 2019 and LACI conclusion meeting on April 21, 2020 from 4-6pm.
- Attend monthly 1-2-hour virtual LACI meetings for the 6-month cohort period: meetings to be held November 2019-March 2020.
- Engage in at least 2 hours of person-to-person collaboration or self-directed learning
- Contribute related resources and insight on the curriculum topic monthly via the virtual platform
- Complete feedback surveys as applicable
Open Call for Abstracts: PFD Research Small Grant Program
Published by Feeding Matters on Sep 02, 2019
- Scientific Reviews – such as systematic, meta-analysis, or scoping; addressing assessment, management, and/or treatment approaches for domains of PFD: medical, nutrition, feeding skill, and psychosocial. The following list offers review suggestions:
- Assessments used in the PFD field (tools, clinician assessments, and/or tests)
- Therapeutic outcomes and/or approaches for PFD treatment
- Resource utilization or economic studies – cost of PFD from the perspective of the healthcare system and/or the family.
Please consider applying using the information below…
General Guidelines and Eligibility:- Funding up to $5,000 for one year from date of award
- No indirect costs or overhead costs
- United States residents
- Methodology must follow PRISMA guidelines
- Open call for abstracts – Friday, September 27, 2019 (by 11:59pm Pacific Time) *new deadline*
- All dates subject to change due to open call deadline extension
- Request for full proposals to be sent to applicants– Wednesday, October 16, 2019
- Full proposal application due – Friday, December 6, 2019 (by 11:59pm Pacific Time)
- Funding and projects begin – Early 2020
- Contact information (name, email, phone number, and mailing address)
- Qualifications & credentials
- Supervising academic mentor (if applicable)
- Funding priority requesting
- Abstract (400-600 words)
- Background
- Research question
- Methodology
- Timeline
For additional information and guidelines, please download the funding guidelines below.

Back to School Time!
Published by Alba Chester on Aug 20, 2019
Infant Allergy Awareness Month
Published by Feeding Matters on Jul 18, 2019
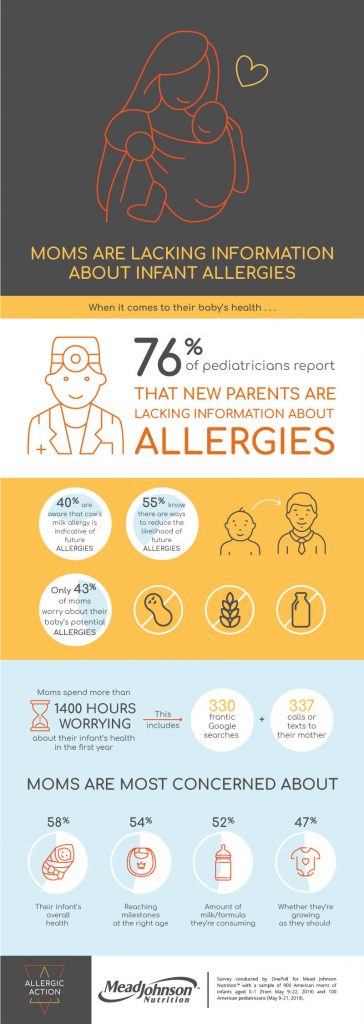 Food allergies in infants and children are becoming more prevalent. A new survey of 900 US moms (of children aged 0-1) and 100 US pediatricians took a look at the issue.
WHEN IT COMES TO THEIR INFANTS’ HEALTH, MOMS ARE WORRIED ABOUT . . .
58% – Their overall health
54% – If they’re reaching milestones at the right age
52% – The amount of milk/formula and/or food they’re consuming
47% – If they’re growing as they should
47% – Their nutritional intake (e.g. vitamins, supplements)
43% – If they have any allergies
41% – The amount of sleep they’re getting
40% – If I’m bonding enough with them
36% – The quality of sleep they’re getting
36% – What their different cries meant
HEALTH ISSUES MOMS HAVE EXPERIENCED IN THEIR INFANTS
54% – Diaper rash
41% – Fever
36% – Cradle cap
34% – Baby acne
32% – Vomiting
30% – Issues breastfeeding
25% – Ear infection
23% – Colic
21% – Allergies
11% – Swollen belly
With 76% of pediatricians reporting that new parents are lacking information about allergies, it’s necessary to stay up-to-date on current treatment and diagnosis information. Health care professionals can learn about the symptoms, diagnoses, and management of food allergies at PNCE.org/food-allergies.
Food allergies in infants and children are becoming more prevalent. A new survey of 900 US moms (of children aged 0-1) and 100 US pediatricians took a look at the issue.
WHEN IT COMES TO THEIR INFANTS’ HEALTH, MOMS ARE WORRIED ABOUT . . .
58% – Their overall health
54% – If they’re reaching milestones at the right age
52% – The amount of milk/formula and/or food they’re consuming
47% – If they’re growing as they should
47% – Their nutritional intake (e.g. vitamins, supplements)
43% – If they have any allergies
41% – The amount of sleep they’re getting
40% – If I’m bonding enough with them
36% – The quality of sleep they’re getting
36% – What their different cries meant
HEALTH ISSUES MOMS HAVE EXPERIENCED IN THEIR INFANTS
54% – Diaper rash
41% – Fever
36% – Cradle cap
34% – Baby acne
32% – Vomiting
30% – Issues breastfeeding
25% – Ear infection
23% – Colic
21% – Allergies
11% – Swollen belly
With 76% of pediatricians reporting that new parents are lacking information about allergies, it’s necessary to stay up-to-date on current treatment and diagnosis information. Health care professionals can learn about the symptoms, diagnoses, and management of food allergies at PNCE.org/food-allergies. Volunteer Spotlight: Amy Delaney
Published by Feeding Matters on Jun 10, 2019
Feeding Matters Volunteer Spotlight is a monthly Q & A series that shares the stories of our growing network of change agents, the driving force behind our vision to create a world where children with pediatric feeding disorder will thrive. This month we bring you Amy Delaney, PHD, SLP.
Amy has been with Feeding Matters since the beginning and currently serves as the lead of our PFD Alliance’s Educational Initiative Committee. She is passionate, dedicated, and her professional knowledge is invaluable to our programs and initiatives. We feel fortunate to have her on our team.
 Tell us a little bit about yourself!
Tell us a little bit about yourself!
I’m an assistant professor in the Department of Speech Pathology and Audiology at Marquette University and director of the Neurodevelopmental Feeding and Swallowing Lab. My research focuses on quantification of age-appropriate feeding practices and defining feeding disorder profiles in children with chronic medical disorders. Some of my ongoing research includes studying typical feeding development in infants and toddlers, standardization of textures and texture progression in childhood, and feeding outcomes in children with congenital heart disease and prematurity. Prior to joining Marquette, I was at the Children’s Hospital of Wisconsin for 20 years as clinician/researcher in pediatric feeding disorder and dysphagia and worked on an interdisciplinary feeding team.
In which volunteer activities have you participated?
Since I started volunteering with the organization in 2007, I’ve assisted in designing content for website, served as co-lead of Feeding Matters’ Pediatric Feeding Disorder (PFD) Dissemination Committee, co-authored the Infant and Child Feeding Questionnaire (ICFQ), presented at the International Pediatric Feeding Disorder Conference (IPFDC), given continuing education workshops, and worked with Feeding Matters’ Founder & Strategic Advisor Shannon Goldwater to develop the provider directory. I’m also a founding and executive council member for the PFD Alliance.
What motivated you to become involved?
I was really drawn to the innovation and passion of Feeding Matters “founding mothers”. I was aligned with their goals and the belief that change and alliance is possible to help children with PFD and their families.
What has been your favorite part of volunteering with Feeding Matters?
I really enjoy the networking, collaboration, and helping the greater good of pediatric feeding. Especially being a part of a global effort with backyard interactions and watching the shear perseverance and persistence of the organization.
What sets Feeding Matters apart from other organizations?
For me, it comes down to three points: the collaborative care model, a focus on improving the care of children and families above all else, and goals are rooted in personal experience and motivation.
The Power of a Name
Published by Feeding Matters on Jul 22, 2019
A smooth, perfectly plump firm apple sits in front of you. The skin is unblemished and the interior is firm and sweet. The seemingly simple task of opening your mouth to take a bite, in actuality, is quite complex. Feeding is the single most complex and physically demanding task an infant will complete for the first few weeks, and even months, of life – requiring the use of 26 muscles and 6 cranial nerves working in perfect harmony to move food and liquid through the body. When one or more pieces of this feeding puzzle are missing, out of order, or unclear, infants and children can have difficulty eating and drinking. That gorgeous apple will remain uneaten.
Although more than 2.3 million children under the age of 5 experience severe pediatric feeding disorder in the United States annually, including 51,000 children in Arizona, PFD often goes undiagnosed and underserved. Like Apollo.
Apollo struggled to feed from birth. His family took him to the doctor again and again, collecting diagnoses including severe reflux, milk allergies, and failure to thrive. He underwent tests for celiac disease and cystic fibrosis. Both came back negative. At 10 months old, he was hospitalized with RSV and pneumonia. He had his adenoids removed. But none of that explained his feeding struggles. By his first birthday, Apollo was skinny, fussy, and still dropping off the growth curve.
For more than 22 months, little Apollo struggled to eat or drink. His mother counted two or three bites as a “good meal”. His doctors were puzzled by his mysterious symptoms. Before Apollo’s family could find the answers they needed, there would be three surgeries, the insertion of a feeding tube, and more than 5 years of feeding treatments.
Fortunately for children like Apollo, the paradigm is shifting. Through the power of a name – pediatric feeding disorder, as published in the Journal of Pediatric Gastroenterology and Nutrition – families navigating the diverse and broad spectrum of pediatric feeding struggles will find the care, support, and resources they need.
But, there’s more work to do. In 2018, Feeding Matters launched a $3 million, 3-year campaign to maximize the efforts needed to launch pediatric feeding disorder, including a $1 million gift from the Dorrance Family Foundation. With your donation, we will accelerate identification, ignite research, and prompt collaborative care for children and families.
That’s the power of a name. [give_form id=”4409″ show_title=”true” show_goal=”true” show_content=”above” display_style=”button” continue_button_title=”Donate Today!”] [give_goal id=”4409″ show_text=”true” show_bar=”true”]

Camp Responsibilities: Establishing Protocols to Prevent and Respond to Food-Allergic Reactions
Published by Food Allergy Research & Education (FARE) on Jun 25, 2019
For the nearly six million children in the U.S. with food allergies, it’s important that camps have established food allergy policies. Food allergy reactions occur without warning and can even occur for the first time while a child, or even a staff member, is at camp.
Having a written food allergy policy in place ensures that staff members are well-equipped to care for anyone who may experience a food allergy reaction while at camp.
Camps should find out whether their state allows them to keep “stock” epinephrine on hand in case someone who has not been previously diagnosed with a food allergy has an allergic reaction. Camp staff should know where epinephrine is stored and be trained on how to administer it.
Creating a Camp Food Allergy Policy
Know about the availability of emergency care, including:
- how to contact emergency medical personnel/ambulance;
- how much time it will take for an emergency crew to arrive;
- how far it is to the nearest hospital; and
- if the hospital has a physician present at all times.
Note that camps in rural settings must understand that ambulance and emergency crews may be volunteers. These emergency situations may require additional plans and medications.
Review the health records submitted by parents and physicians.
- This includes the Food Allergy & Anaphylaxis Emergency Care Plan. Ask questions if you do not understand anything in these documents.
Establish prevention protocols for your camp.
- Be certain that all food service or kitchen personnel are aware of, and can identify, campers with food allergies.
- Discuss meal plans with parents and the camper. Make alternative plans if necessary.
- Plan how a camper with food allergies will take part in meals. For example, he or she might need to go first in a buffet line and at other food-related events to avoid cross-contact. Or, the camper might need to sit apart from other campers, in a special allergen-free space. In the latter case, try to have someone sit with the camper so he or she doesn’t feel excluded.
- Make sure that all staff can recognize the symptoms of an allergic reaction and know what to do if a reaction occurs.
- Maintain an appropriate sense of confidentiality and respect for individual privacy.
- Make sure the nurse has the required authorizations and appropriate medications to use in the event of accidental contact or ingestion.
Ensure that appropriate personnel are familiar with how to use epinephrine, where the medication is located and the camp protocol.
- Schedule a training session before the start of camp. Allow participants to become familiar with how to operate the different types of epinephrine auto-injectors.
- Comply with local and state regulations about the administration of medication.
Plan for field trips or offsite activities.
- Be certain any emergency medications and authorizations go with the camper and staff.
- On trips away from the camp, staff should always carry a communication device (e.g., cell phone, two-way radio).
- Some medications, such as epinephrine, become ineffective if exposed to temperature extremes (heat or cold) or light. Be certain that all personnel understand the importance of keeping medication protected.
For additional information and resources on creating a safe and positive experience for campers with food allergies, visit FARE’s camp web page.

Summer Travel Tips for Children with Special Needs
Published by Cathy Humphrey on Jun 05, 2019
- Planning
Whether you’re going on a day trip or a multi-day vacation of your dreams —planning is key! Where are you going? What will you be doing and do you need to make special arrangements? How long will you stay? What resources will you need (Special foods? Medical equipment? Vehicle rental? Accessible transportation between the airport and hotel?). brettapproved is a useful source for accessible hotels, restaurants, and entertainment venues.
American Airlines also has a program that was created for children with autism and other special needs. It’s Cool to Fly American is a mock travel experience where children and their families can experience the airport before traveling. The 3 ½ hour experience includes parking, check in, waiting at the gate, boarding a plane, taxing, returning to the gate, and retrieving their luggage. - Preparation
Making lists is necessary for a successful vacation, especially when traveling with people who have special feeding or other healthcare needs. Lists are part of planning and part of preparation. An itinerary that includes key contacts, phone numbers, and addresses is useful. A list of what to pack (you can make a list for each person traveling or just for the person with special healthcare needs) is very important—starting with items you can’t buy where you’re going, such as medicine and special foods. You can be as general or detailed as you need (toiletries and food OR 6 diapers and 4 pull ups per day x 8 days, 2 packets of x food, 3 packets of food, 2 spoons, 1 dish), but I find it helps the planning and preparation process to include every last item!
Preparation also includes being ready for “What if” questions. What if her g-tube falls out? (Include “spare g-tube” on list.) What if we can’t find pureed foods where we’re going? (Decide how many packets of food to bring or find nearby grocery stores.) What if he has a medical emergency and we need his latest scans or medical records? (Bring CDs of critical scans and usernames/ passwords for electronic medical records or put copies of important records in Dropbox, Google Folder, or other cloud-based location.) What if she needs to go to the emergency room? (Include the address to the nearest children’s hospital to your destination on your list.) And so on.
If you are going to Disney World, there is a discussion group on Facebook called Meals & Wheels in Disney World for people with questions about food allergies, wheelchairs, and pureed food. The creator of the group is a travel agent and has two kids with special healthcare needs. Preparation is a key component of a successful vacation. - Flexibility
Another key component is flexibility — especially when travelling with a person who has special healthcare needs. Like preparation, flexibility starts during planning and continues until you arrive back home. Let’s say you want to take your family on safari in Africa, but your child doesn’t travel well or you’re not sure if the menu has pureed foods to feed your child with pediatric feeding disorder. When you’re flexible, rather than seeing an obstacle, you see opportunities – bring your own food or a blender, talk with the travel company or the chef, go somewhere else, or start by driving up the road to a nearby wildlife or ammusement park! You may be comfortable with some flexibility in day-to-day activities, but it’s especially important when on vacation with a child that has special healthcare needs! - Sense of Humor
In addition to flexibility, having a sense of humor helps you have a successful holiday. When things happen on vacation – and they will – you have a choice: you can let it ruin your trip, or you can laugh about it. When the sixth person in a row tells you how to feed your child with PFD, or when the hotel room is so small you can’t fit the wheelchair inside, you can scream and rant or you can see it as a teaching opportunity. Explain what PFD is and why feeding your child is not the same as when they were feeding their children. Smile when you show the front desk clerk photos of your family member not being able to get in the room and ask for an upgrade. - Choose Love not Fear
Finally, when deciding whether or not to travel with a child that has special healthcare needs, choose love not fear. Go for it! Take that vacation! Heck, start small by going on a staycation, see how it goes and build from there. Going on a cruise is a great choice because they are typically very accessible (be sure to reserve an accessible cabin if someone in your party has a wheelchair) and the food choices are varied and flexible. All-inclusive resorts are also a good choice if you want a variety of activities and meals included without leaving the property. Car trips might be better than plane trips if you need to bring lots of equipment.
Whatever you do, don’t be afraid to go out and have fun because you’re fearful of what others might say or do, or that you won’t be able to find the right food or a changing station for your teenage child. Plan. Prepare. Try new things. Smile. Laugh. Make memories. Maybe we’ll see you out there!
Volunteer Spotlight: Leslie Jackson
Published by Feeding Matters on Jul 09, 2019
Leslie is one of our Power of Two family coaches in Texas. Leslie’s journey with her son Jacob first brought her to Feeding Matters as a parent needing support. Now, she helps families navigate their journey with PFD by offering her insight, empathy, and compassion.
 Tell us a little bit about yourself!
Tell us a little bit about yourself!I am a graduate student studying to receive a master’s degree in social work. I am interning at a children’s charity and am lucky to work to support families of children with special needs. I live in Austin, Texas with my husband, ten-year-old son, and three cats. When my husband and I met- I had two cats and he had one- so we became a three-cat family!
How long have you been a volunteer with Feeding Matters?
I have been a volunteer with Feeding Matters since the spring of 2017.
In which volunteer activities have you participated?
I am a Power of Two coach for families who are experiencing feeding challenges with their child.
 What motivated you to become involved?
What motivated you to become involved?My son was born as a micro preemie, weighing 1 pound, 13 ounces. He spent four months in the NICU. He was medically fragile and failure to thrive for his first three years. He has severe reflux and oral aversions. I remember feeling very isolated with my son’s feeding challenges and not knowing where to turn for support. I volunteer to help ensure other families experiencing feeding difficulties have support.
What has been your favorite part of volunteering with Feeding Matters?
I have been inspired by the strength and resilience of the families and children I have been fortunate enough to get to know as a Feeding Matters Family Coach.
What sets Feeding Matters apart from other organizations?
Feeding Matters understands how challenging it can be for parents of children with PFD to find support! The education and support provided by Feeding Matters is truly unique and a gift to so many.